Illness Perceptions and Response to Treatment with Romiplostim in Iraqi Patients with Refractory Immune Thrombocytopenia Purpura: A Cross-Sectional Study
DOI:
https://doi.org/10.54133/ajms.v9i2.2435الكلمات المفتاحية:
Immune thrombocytopenic purpura، Illness perception، Romiplostimالملخص
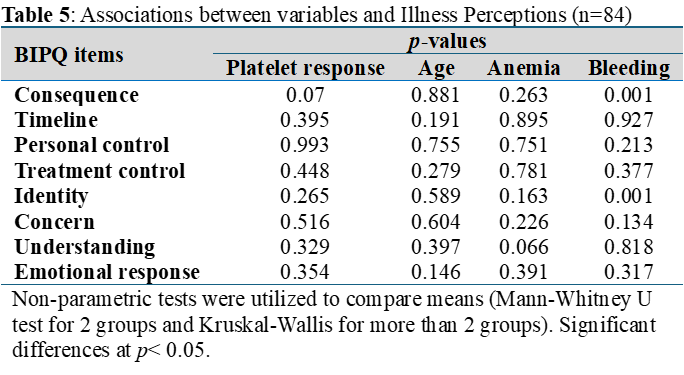
Background: Immune thrombocytopenia is an immune-related disorder that causes an impairment in platelet production and stimulates platelet destruction, causing variable bleeding symptoms. Objective: This study focuses on refractory immune thrombocytopenic purpura patients on romiplostim treatment and their level of illness perception related to treatment response. Method: A cross-sectional study was conducted from May 1st, 2025, to August 1st, 2025. Brief Illness Perception Questionnaires were administered to 84 patients with ITP to collect the data. The study took place at the Hematology and Bone Marrow Transplant Center, Medical City, Baghdad, Iraq. Results: The romiplostim response rate is 21 (25.0%), while the partial response rate is 41 (48.8%). The most frequent complaints were bleeding, 46 (54.8%), and joint pain, 30 (35.7%). In terms of illness perceptions, treatment control had the greatest mean score (6.9±2.85), and understanding had the lowest mean score (4.2±4.6). Conclusions: Romiplostim showed effective management among Iraqi patients, and the patients believe in its effectiveness. A low level of patient understanding was shown among the participants; education programs and patient counseling are required to increase health literacy among patients with immune thrombocytopenic purpura.
التنزيلات
المراجع
Cooper N, Ghanima W. Immune thrombocytopenia. N Engl J Med. 2019;381(10):945-955. doi: 10.1056/NEJMcp1810479. DOI: https://doi.org/10.1056/NEJMcp1810479
Fogarty PF. Chronic immune thrombocytopenia in adults: epidemiology and clinical presentation. Hematol Oncol Clin North Am. 2009;23(6):1213-1221. doi: 10.1016/j.hoc.2009.08.004. DOI: https://doi.org/10.1016/j.hoc.2009.08.004
Consolini R, Legitimo A, Caparello MC. The centenary of immune thrombocytopenia–part 1: revising nomenclature and pathogenesis. Front Pediatr. 2016;4:102. doi: 10.3389/fped.2016.00102. DOI: https://doi.org/10.3389/fped.2016.00102
Olsson B, Andersson PO, Jernås M, Jacobsson S, Carlsson B, Carlsson LM, et al. T-cell-mediated cytotoxicity toward platelets in chronic idiopathic thrombocytopenic purpura. Nat Med. 2003;9(9):1123-1124. doi: 10.1038/nm921. DOI: https://doi.org/10.1038/nm921
Chang M, Nakagawa PA, Williams SA, Schwartz MR, Imfeld KL, Buzby JS, et al. Immune thrombocytopenic purpura (ITP) plasma and purified ITP monoclonal autoantibodies inhibit megakaryocytopoiesis in vitro. Blood. 2003;102:887‑895. doi: 10.1182/blood-2002-05-1475. DOI: https://doi.org/10.1182/blood-2002-05-1475
McMillan R, Wang L, Tomer A, Nichol J, Pistillo J. Suppression of in vitro megakaryocyte production by antiplatelet autoantibodies from adult patients with chronic ITP. Blood. 2004;103:1364‑1369. doi: 10.1182/blood-2003-08-2672. DOI: https://doi.org/10.1182/blood-2003-08-2672
Houwerzijl EJ, Blom NR, van der Want JJ, Esselink MT, Koornstra JJ, Smit JW, et al. Ultrastructural study shows morphologic features of apoptosis and para‑apoptosis in megakaryocytes from patients with idiopathic thrombocytopenic purpura. Blood. 2004;103:500‑506. doi: 10.1182/blood-2003-01-0275. DOI: https://doi.org/10.1182/blood-2003-01-0275
Zhang F, Chu X, Wang L, Zhu Y, Li L, Ma D, et al. Cell‑mediated lysis of autologous platelets in chronic idiopathic thrombocytopenic purpura. Eur J Haematol. 2006;76:427‑431. doi: 10.1111/j.1600-0609.2005.00622.x. DOI: https://doi.org/10.1111/j.1600-0609.2005.00622.x
Janeway CA, (Ed.), The Humoral Immune Response. In: Immunobiology: The Immune System in Healthand Disease, (5th edn.), U.S. National Library of Medicine, 1 Jan. 1970. (PDF) Difference Between Humoral and Cell Mediated Immunity. Available from: https://www.researchgate.net/publication/320180727_Difference_Between_Humoral_and_Cell_Mediated_Immunity#fullTextFileContent
Ellithy HN, Yousry SM, Abdel-Aal A, Tawadros L, Momen N. Association of CD40 gene polymorphisms and immune thrombocytopenic purpura in the adult Egyptian population. Blood Res. 2022;57(3):229-234. doi: 10.5045/br.2022.2022057. DOI: https://doi.org/10.5045/br.2022.2022057
Shanshal AM, Mohammed SI, Matti BF. CD40 gene variants and disease susceptibility: A comprehensive review of associations with immune-mediated inflammatory diseases, cancer, and infectious diseases. Al-Rafidain J Med Sci. 2025;8(2):114-121. doi: 10.54133/ajms.v8i2.1904. DOI: https://doi.org/10.54133/ajms.v8i2.1904
Provan D, Arnold DM, Bussel JB, Chong BH, Cooper N, Gernsheimer T, et al. Updated international consensus report on the investigation and management of primary immune thrombocytopenia. Blood Adv. 2019;3(22):3780–3817. doi: 10.1182/bloodadvances.2019000812. DOI: https://doi.org/10.1182/bloodadvances.2019000812
Gernsheimer T, Stratton J, Ballem PJ, Slichter SJ. Mechanisms ofresponse to treatment in autoimmune thrombocytopenic purpura. N Engl J Med. 1989;320(15):974–980. doi: 10.1056/NEJM198904133201505. DOI: https://doi.org/10.1056/NEJM198904133201505
Kitchens CS. Amelioration of endothelial abnormalities by predni-sone in experimental thrombocytopenia in the rabbit. J Clin Invest.1977;60(5):1129-1134. doi: 10.1172/JCI108864. DOI: https://doi.org/10.1172/JCI108864
Guidry JA, George JN, Vesely SK, Kennison SM, Terrell DR. Corticosteroid side- effects and risk for bleeding in immune thrombocytopenic purpura: patient and hematologist perspectives. Eur J Haematol. 2009;83(3):175-182. doi: 10.1111/j.1600- 0609.2009.01265.x. DOI: https://doi.org/10.1111/j.1600-0609.2009.01265.x
Provan D, Stasi R, Newland AC, Blanchette VS, Bolton-Maggs P, Bussel JB, et al. International consensus report on the investigation and management of primary immune thrombocytopenia. Blood. 2010;115(2):168-186. doi: 10.1182/blood-2009-06-225565. DOI: https://doi.org/10.1182/blood-2009-06-225565
Matzdorff A, Meyer O, Ostermann H, Kiefel V, Eberl W, Kühne T, et al. Immune thrombocytopenia - Current diagnostics and therapy: recommendations of a joint working group of DGHO, ÖGHO, SGH, GPOH, and DGTI. Oncol Res Treat. 2018;41(Suppl 5):1–30. doi: 10.1159/000492187. DOI: https://doi.org/10.1159/000492187
Lozano ML, Sanz MA, Vicente V. Guidelines of the Spanish ITP Group for the diagnosis, treatment and follow-up of patients with immune thrombopenia. Med Clin (Barc). 2021;157(4):191-198. doi: 10.1016/j.medcli.2021.03.017. DOI: https://doi.org/10.1016/j.medcle.2021.07.003
Marshall AL, Scarpone R, De Greef M, Bird R, Kuter DJ. Remissions after long-term use of romiplostim for immunethrombocytopenia. Haematologica. 2016;101(12):476-478. doi: 10.3324/haematol.2016.151886. DOI: https://doi.org/10.3324/haematol.2016.151886
Wong RSM, Saleh MN, Khelif A, Salama A, Portella MSO, Burgess P, et al. Safety and efficacy of long-term treatmentof chronic/persistent ITP with eltrombopag: final results of the EXTEND study. Blood. 2017;130(23):2527-2536. doi: 10.1182/blood-2017-04-748707. DOI: https://doi.org/10.1182/blood-2017-04-748707
Al-Samkari H, Nagalla S. Efficacy and safety evaluation of ava-trombopag in immune thrombocytopenia: analyses of a phase III study and long-term extension. Platelets. 2022;33(2):257-264. doi: 10.1080/09537104.2021.1881952. DOI: https://doi.org/10.1080/09537104.2021.1881952
Neunert C, Terrell DR, Arnold DM, Buchanan G, Cines DB, Cooper N, et al. American Society of Hematology 2019 guidelines for immune thrombocytopenia. Blood Adv. 2019;3(23):3829–3866. doi: 10.1182/bloodadvances.2019000966. DOI: https://doi.org/10.1182/bloodadvances.2019000966
Popiołek L, Dzieża-Grudnik A, Siga O, Popiołek I, Moląg M, Królczyk J, et al. Coping with stress and hypertension-mediated organ damage. Arch Psychiatry Psychother. 2019;21(4):27–36. doi: 10.12740/APP/108666. DOI: https://doi.org/10.12740/APP/108666
Shakya R, Shrestha S, Gautam R, Rai L, Maharjan S, Satyal GK, et al. Perceived illness and treatment adherence to hypertension among patients attending a tertiary hospital in Kathmandu, Nepal. Patient Prefer Adher. 2020;14:2287–300. doi: 10.2147/PPA.S270786. DOI: https://doi.org/10.2147/PPA.S270786
Mjali A, Matti BF, Abbas NT, Nassrullah HA, Naji AS, Alwan AF, et al. Do we need local guidelines for the diagnosis and management of immune thrombocytopenia in Iraq? J Appl Hematol. 2023;14(2):146-156. doi: 10.4103/joah.joah_7_23 DOI: https://doi.org/10.4103/joah.joah_7_23
Goshua G, Sinha P, Kunst N, Pischel L, Lee AI, Cuker A. Cost‐effectiveness of second‐line therapies in adults with chronic immune thrombocytopenia. Am J Hematol. 2023;98(1):122-130. doi: 10.1002/ajh.26497. DOI: https://doi.org/10.1002/ajh.26497
Neunert C, Lim W, Crowther M, Cohen A, Solberg L, Crowther MA. American Society of Hematology. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. Blood. 2011;117(16):4190–4207. doi: 10.1182/blood-2010-08-302984. DOI: https://doi.org/10.1182/blood-2010-08-302984
Romiplostim, Prescribing Information. Thousand Oaks, CA: Amgen; 2008.
Williams AM, Ansai N, Ahluwalia N, Nguyen DT. Anemia Prevalence: United States, August 2021-August 2023. doi: 10.15620/cdc/168890. DOI: https://doi.org/10.15620/cdc/168890
US Department of Health and Human Services. Common terminology criteria for adverse events (CTCAE). (No Title). 2017 Nov 27.27. US Department of Health and Human Services, National Institutes of Health, National Cancer Institute.
Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60(6):631-637. doi: 10.1016/j.jpsychores.2005.10.020. DOI: https://doi.org/10.1016/j.jpsychores.2005.10.020
Saarti S, Jabbour H, El Osta N, Hajj A, Khabbaz LR. Cross-cultural adaptation and psychometric properties of an Arabic language version of the brief illness perception questionnaire in Lebanon. Libyan J Med. 2016;11(1):31976. doi: 10.3402/ljm.v11.31976. DOI: https://doi.org/10.3402/ljm.v11.31976
Alaa R. Prevalence of immune thrombocytopenia purpura in Wasit province. Wasit J Pure Sci. 2024;3(3):160-164. doi: 10.31185/wjps.455. DOI: https://doi.org/10.31185/wjps.455
Talfah AM, Badwan SA, AL-Halalmeh AI, Khawaldeh MH, Obeidat MA. Comparison of treatment regimens used in patients diagnosed with idiopathic thrombocytopenic purpura. JRMS. 2019;26(2):24-32. doi: 10.12816/0053288. DOI: https://doi.org/10.12816/0053288
Al-Zahrani H, Aleem A, Mohareb FA, Ahmed SY, Al-Suliman AM, Al Saeed HH, et al. Management of adult immune thrombocytopenia: Recommendations by an expert Saudi panel. J Appl Hematol. 2019;10(3):77-83. doi: 10.4103/joah.joah_51_19. DOI: https://doi.org/10.4103/joah.joah_51_19
Jumaa AK, Saleh TA, Khalaf AA, Abbas MS. Efficacy and safety of romiplostim in adult Iraqi patients with refractory immune thrombocytopenia. Iraqi J Hematol. 2020;9(2):92-96. doi: 10.4103/ijh.ijh_21_20. DOI: https://doi.org/10.4103/ijh.ijh_21_20
Anwer IY, Yawuz MJ, Al-Jumaili AA. In-depth assessment of Iraqi physicians' adherence to treatment guidelines for different diseases: a qualitative study. F1000Research. 2024;12(350):350. doi: 10.12688/f1000research.128233.1.
Snell Taylor SJ, Nielson CM, Breskin A, Saul B, Yu Y, Alam N, et al. Effectiveness and safety of romiplostim among patients with newly diagnosed, persistent and chronic immune thrombocytopenia in European clinical practice. Adv Ther. 2021;38(5):2673-2688. doi: 10.1007/s12325-021-01727-5. DOI: https://doi.org/10.1007/s12325-021-01727-5
Anwer IY, Yawuz MJ, Al-Jumaili AA. In-depth assessment of Iraqi physicians' adherence to treatment guidelines for different diseases: a qualitative study. F1000Research. 2024;12(350):350. doi: 10.12688/f1000research.128233.1. DOI: https://doi.org/10.12688/f1000research.128233.2
Shanshal AM, Ataimish AH. Evaluation of knowledge, attitudes and experience of off-label drug prescribing practice among physicians in Baghdad city hospitals. Iraqi J Pharm Sci. 2019;28(2):115-123. doi: 10.31351/vol28iss2pp115-123. DOI: https://doi.org/10.31351/vol28iss2pp115-123
Gardiner EE, Thom JY, Al-Tamimi M, Hughes A, Berndt MC, Andrews RK, et al. Restored platelet function after romiplostim treatment in a patient with immune thrombocytopenic purpura Br J Haematol. 2010;149:625–628. doi: 10.1111/j.1365-2141.2010.08092.x. DOI: https://doi.org/10.1111/j.1365-2141.2010.08092.x
Hanson SR, Slichter SJ. Platelet kinetics in patients with bone marrow hypoplasia: evidence for a fixed platelet requirement. Blood. 1985;66(5):1105-1109. doi: 10.1182/blood.V66.5.1105.bloodjournal6651105. DOI: https://doi.org/10.1182/blood.V66.5.1105.bloodjournal6651105
Schoonen WM, Kucera G, Coalson J, Li L, Rutstein M, Mowat F, et al. Epidemiology of immune thrombocytopenic purpura in the General Practice Research Database. Br J Haematol. 2009;145(12):235–244. doi: 10.1111/j.1365-2141.2009.07615.x. DOI: https://doi.org/10.1111/j.1365-2141.2009.07615.x
Portielje JE, Westendorp RG, Kluin-Nelemans HC, Brand A. Morbidity and mortality in adults with idiopathic thrombocytopenic purpura. Blood. 2001;97(9):2549–2554. doi: 10.1182/blood.v97.9.2549. DOI: https://doi.org/10.1182/blood.V97.9.2549
Nørgaard M, Jensen AO, Engebjerg MC, Farkas DK, Thomsen RW, Cha S, et al. Long-term clinical outcomes of patients with primary chronic immune thrombocytopenia: a Danish population-based cohort study. Blood. 2011;117:3514–3520. doi: 10.1182/blood-2010-10-312819. DOI: https://doi.org/10.1182/blood-2010-10-312819
Schattner E, Bussel J. Mortality in immune thrombocytopenic purpura: Report of seven cases and consideration of prognostic indicators. Am J Hematol. 1994;46:120-126. doi: 10.1002/ajh.2830460212. DOI: https://doi.org/10.1002/ajh.2830460212
Cohen YC, Djulbegovic B, Shamai-Lubovitz O, Mozes B. The bleeding risk and natural history of idiopathic thrombocytopenic purpura in patients with persistent low platelet counts. Arch Intern Med. 2000;160(11):1630-1638. doi: 10.1001/archinte.160.11.1630. DOI: https://doi.org/10.1001/archinte.160.11.1630
Rasu RS, Bawa WA, Suminski R, Snella K, Warady B. Health literacy impact on National Healthcare Utilization and expenditure. Int J Health Policy Manag. 2015;4(11):747–755. doi: 10.15171/ijhpm.2015.151. DOI: https://doi.org/10.15171/ijhpm.2015.151
Al-Nema ZM. Comparison of health literacy among Iraqi women with different age groups. Asian J Pharm Clin Res. 2018;11(2):1-3. doi: 10.22159/ajpcr.2018.v11i2.22707. DOI: https://doi.org/10.22159/ajpcr.2018.v11i2.22707
Al-Mandalawi RT, Al-Metwali BZ, Gorial FI. Impact of pharmacist-led intervention on adherence, quality of life, and self-efficacy among Iraqi patients with systemic lupus erythematosus. Al-Rafidain J Med Sci. 2025;8(2):224-230. doi: 10.54133/ajms.v8i2.2038. DOI: https://doi.org/10.54133/ajms.v8i2.2038
Mohammed SI, Dawood EB, Abaas IS. Perceptions and attitudes of community pharmacists towards patient counseling and continuing pharmacy education programs in Iraq. Iraqi J Pharm Sci. 2019;28(2):30-36. doi.: 10.31351/vol28iss2pp30-36. DOI: https://doi.org/10.31351/vol28iss2pp30-36
التنزيلات
منشور
كيفية الاقتباس
إصدار
القسم
الرخصة
الحقوق الفكرية (c) 2025 Al-Rafidain Journal of Medical Sciences

هذا العمل مرخص بموجب Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).










