Immunohistochemical Expression of CD47 and Signal Regulatory Protein-α in B-Cell Lymphoma
DOI:
https://doi.org/10.54133/ajms.v9i2.2430Keywords:
B Lymphoma, CD47Abstract
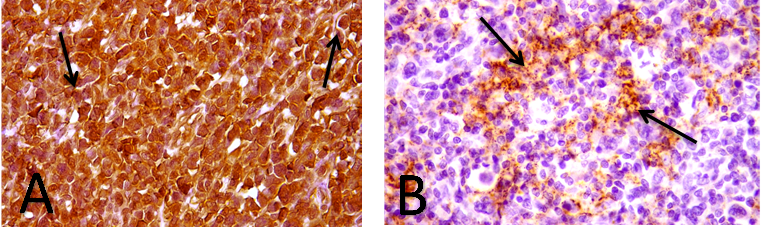
Background: Lymphoma is one of many tumors that develop mechanisms to avoid the immune system. One mechanism of immune system evasion is CD47 interaction with various ligands, including signal regulatory protein alpha (SIRP-α). This interaction inhibits phagocytosis of lymphoma cells. Objectives: To assess and compare the frequency of combined immunohistochemical expression of CD47 and SIRP-α in B cell lymphomas in addition to studying its association with some clinicopathological parameters. Methods: A retrospective and prospective case series study of 51 cases of B-cell lymphomas collected randomly from the histopathological department of governmental and some private laboratories in Nineveh Province over a period of six months extending from September 2024 to February 2025. An immunohistochemistry investigation using CD47 and SIRP-α was performed, and the positive expression data were evaluated. Results: The mean age was 31.29 years for HL and 62 years for NHL, with slight male predominance (51%) and (66.67%) had nodal presentation. B-cell lymphoma cases included in this study show immunohistochemical expression of CD47 and SIRP-α, but with different staining grades. 64.71% and 33.33% were high expressors vs. 35.29% and 66.67% were low expressors for CD47 and SIRPA, respectively, with no significant association. Conclusions: Although CD47 and SIRPα showed divergent results, this study revealed that most B-cell lymphomas express CD47 and SIRPα proteins independently.
Downloads
References
Ennishi D, Hsi ED, Steidl C, Scott DW. Toward a new molecular taxonomy of diffuse large B-cell lymphoma. Cancer Discov. 2020;10(9):1267-1281. doi: 10.1158/2159-8290.CD-19-1444. DOI: https://doi.org/10.1158/2159-8290.CD-20-0174
Storck K, Brandstetter M, Keller U, Knopf A. Clinical presentation and characteristics of lymphoma in the head and neck region. Head Face Med. 2019;15(1):1. doi: 10.1186/s13005-018-0186-0. DOI: https://doi.org/10.1186/s13005-018-0186-0
Ansell SM. Hodgkin lymphoma: 2023 update on diagnosis, risk-stratification, and management. Am J Hematol. 2022;97(11):1478-1488. doi: 10.1002/ajh.26674. DOI: https://doi.org/10.1002/ajh.26717
Weniger MA, Küppers R. Molecular biology of Hodgkin lymphoma. Leukemia. 2021;35(4):968–981. doi: 10.1038/s41375-021-01204-6. DOI: https://doi.org/10.1038/s41375-021-01204-6
Kshatri JS, Satpathy P, Sharma S, Bhoi T, Mishra SP, Sahoo SS. Health research in the state of Odisha, India: a decadal bibliometric analysis (2011–2020). J Family Med Prim Care. 2022;11(7):3771–3776. doi: 10.4103/jfmpc.jfmpc_2192_21. DOI: https://doi.org/10.4103/jfmpc.jfmpc_2192_21
Singh R, Shaik S, Negi BS, Rajguru JP, Patil PB, Parihar AS, et al. Non-Hodgkin’s lymphoma: a review. J Family Med Prim Care. 2020;9(4):1834-1840. doi: 10.4103/jfmpc.jfmpc_1037_19. DOI: https://doi.org/10.4103/jfmpc.jfmpc_1037_19
Thandra KC, Barsouk A, Saginala K, Padala SA, Barsouk A, Rawla P. Epidemiology of non-Hodgkin’s lymphoma. Med Sci (Basel). 2021;9(1):5. doi: 10.3390/medsci9010005. DOI: https://doi.org/10.3390/medsci9010005
Zafar S, Sharma RK, Cunningham J, Mahalingam P, Attygalle AD, Khan N, et al. Current and future best practice in imaging, staging, and response assessment for non-Hodgkin’s lymphomas: the SIHMIR paradigm shift. Clin Radiol. 2021;76(5):391.e1-18. doi: 10.1016/j.crad.2020.12.022. DOI: https://doi.org/10.1016/j.crad.2020.12.022
Abou Dalle I, Dulery R, Moukalled N, Ricard L, Stocker N, El-Cheikh J, et al. Bi- and tri-specific antibodies in non-Hodgkin lymphoma: current data and perspectives. Blood Cancer J. 2024;14(1):23. doi: 10.1038/s41408-024-00989-w. DOI: https://doi.org/10.1038/s41408-024-00989-w
Patel HS, Shah S, Goswami HM. Role of immunohistochemistry in differential diagnosis of lymphoma (A study of 200 cases). Int J Contemp Pathol. 2020;6(1). doi: 10.18203/2320-6012.ijcpath20200850.
Zuhair Z, Khattab KW. The utility of CD10 and MUM1 immunohistochemical stains in subtyping diffuse large B-cell lymphoma. J Nat Sci Biol Med. 2024;15(1):51–57. doi: 10.4103/jnsbm.JNSBM_15_1_6.
Alshahwany MA, Kachachi MS, Jawhar NM. Immunohistochemical expression of PD-L1 and EBV in Hodgkin’s lymphoma. Ann Coll Med Mosul. 2024;46(1):6–10. doi: 10.33899/mmed.2024.146119.1249. DOI: https://doi.org/10.33899/mmed.2024.146119.1249
Mohammed JZ, Khattab KW. BCL6 immunohistochemical expression in diffuse large B-cell lymphoma. Ann Coll Med Mosul. 2024;46(1):43-48. doi: 10.33899/mmed.2024.145600.1245. DOI: https://doi.org/10.33899/mmed.2024.145600.1245
Al-Taee ZA, Zamil RH, Al-Kattan SD, Al-Kaabi MM, Kamal AM. Distribution of lymphoma cases and significance of diagnostic immunohistochemistry in a sample of Iraqi patients: a cross-sectional study in a tertiary center in Baghdad. Al-Rafidain J Med Sci. 2025;8(2):242-248. doi: 10.54133/ajms.v8i2.1960. DOI: https://doi.org/10.54133/ajms.v8i2.1960
Eladl E, Tremblay-LeMay R, Rastgoo N, Musani R, Chen W, Liu A, et al. Role of CD47 in hematological malignancies. J Hematol Oncol. 2020;13:96. doi: 10.1186/s13045-020-00930-1. DOI: https://doi.org/10.1186/s13045-020-00930-1
Huang CY, Ye ZH, Huang MY, Lu JJ. Regulation of CD47 expression in cancer cells. Transl Oncol. 2020;13(12):100862. doi: 10.1016/j.tranon.2020.100862. DOI: https://doi.org/10.1016/j.tranon.2020.100862
Yang H, Xun Y, You H. The landscape overview of CD47-based immunotherapy for hematological malignancies. Biomark Res. 2023;11(1):15. doi: 10.1186/s40364-023-00456-x. DOI: https://doi.org/10.1186/s40364-023-00456-x
Huang J, Liu F, Li C, Liang X, Li C, Liu Y, et al. Role of CD47 in tumor immunity: a potential target for combination therapy. Sci Rep. 2022;12(1):9803. doi: 10.1038/s41598-022-13764-3. DOI: https://doi.org/10.1038/s41598-022-13764-3
Logtenberg MEW, Scheeren FA, Schumacher TN. The CD47–SIRPα immune checkpoint. Immunity. 2020;52(5):742–752. doi: 10.1016/j.immuni.2020.04.011. DOI: https://doi.org/10.1016/j.immuni.2020.04.011
Maute R, Xu J, Weissman IL. CD47–SIRPα-targeted therapeutics: status and prospects. Immuno-Oncol Technol. 2022;13:100070. doi: 10.1016/j.iotech.2022.100070. DOI: https://doi.org/10.1016/j.iotech.2022.100070
Yang K, Xu J, Liu Q, Li J, Xi Y. Expression and significance of CD47, PD1 and PDL1 in T-cell acute lymphoblastic lymphoma/leukemia. Pathol Res Pract. 2019;215(2):265–2671. doi: 10.1016/j.prp.2018.10.021. DOI: https://doi.org/10.1016/j.prp.2018.10.021
Dizman N, Buchbinder EI. Cancer therapy targeting CD47/SIRPα. Cancers (Basel). 2021;13(24):6229. doi: 10.3390/cancers13246229. DOI: https://doi.org/10.3390/cancers13246229
Kazama R, Miyoshi H, Takeuchi M, Miyawaki K, Nakashima K, Yoshida N, et al. Combination of CD47 and signal-regulatory protein-α constituting the “don’t eat me” signal is a prognostic factor in diffuse large B-cell lymphoma. Cancer Sci. 2020;111(7):2608–2619. doi: 10.1111/cas.14448. DOI: https://doi.org/10.1111/cas.14437
Khalil MA, Dagash MT, Al-Essawi AJ. Association of Epstein–Barr virus (EBV) with development of Hodgkin lymphoma in western region of Iraq: unmatched molecular case–control study. Indian J Forensic Med Toxicol. 2020;14(2). doi: 10.21203/rs.3.rs-107968/v1.
Mohammedzaki LB, Hasan KM, Polus RK, Yassin AK. Clinicopathological, immunohistochemical characteristics and the outcome of Hodgkin lymphoma patients in Erbil city, Iraq. Iraqi J Hematol. 2019;8(1):14-20. doi: 10.4103/ijh.ijh_8_19. DOI: https://doi.org/10.4103/ijh.ijh_18_18
Monabati A, Safaei A, Noori S, Mokhtari M, Vahedi A. Subtype distribution of lymphomas in South of Iran, analysis of 1085 cases based on World Health Organization classification. Ann Hematol. 2016;95(4):613-618. doi: 10.1007/s00277-016-2592-0. DOI: https://doi.org/10.1007/s00277-016-2590-5
Aljufairi EA, George SM, Alshaikh SA, Radhi AA, Mohamed RM. Spectrum of lymphoma in Bahrain: A retrospective analysis according to the World Health Organization classification. Saudi Med J. 2018;39(7):736-741. doi: 10.15537/smj.2018.7.22297. DOI: https://doi.org/10.15537/smj.2018.7.23065
Harahap AS, Charles S, Ham MF, Ham M. A decade of prevalence and clinicopathological insights into classical Hodgkin lymphoma: A study from an Indonesian tertiary hospital. Cureus. 2024;16(11):e7056. doi: 10.7759/cureus.7056. DOI: https://doi.org/10.7759/cureus.73482
Aslani A, Morsali S, Mousavi SE, Choupani S, Yekta Z, Nejadghaderi SA. Adult Hodgkin lymphoma incidence trends in the United States from 2000 to 2020. Sci Rep. 2024;14(1):20500. doi: 10.1038/s41598-024-20500-8. DOI: https://doi.org/10.1038/s41598-024-69975-3
Huang J, Chan SC, Lok V, Zhang L, Lucero-Prisno DE, Xu W, et al. Global burden, risk factors, and trends of non-Hodgkin lymphoma: A worldwide analysis of cancer registries. Cancer Med. 2024;13(5):e7056. doi: 10.1002/cam4.7056. DOI: https://doi.org/10.1002/cam4.7056
Touma E, Antoun L, Hallit S, Nasr F, Massoud M, El Othman R, et al. Non-Hodgkin lymphoma in Lebanon: a retrospective epidemiological study between 1984 and 2019. BMC Public Health. 2021;21:2218. doi: 10.1186/s12889-021-12276-8. DOI: https://doi.org/10.1186/s12889-021-11840-3
Dogan A, Doğan NY, Erkurt MA, Ekinci Ö, Kuku İ, Kaya E. Clinical and pathological characteristics of patients with non-Hodgkin lymphoma in Eastern Turkey. Cukurova Med J. 2020;45(2):533-540. doi: 10.17826/cumj.709774. DOI: https://doi.org/10.17826/cumj.672199
Alyahya N, Adiga B, Alwadei A, Alshahrani G, Alyahya F. The clinico-pathological profile of non-Hodgkin’s lymphoma in Aseer region of Saudi Arabia. BMC Res Notes. 2019;12:789. doi: 10.1186/s13104-019-4823-4. DOI: https://doi.org/10.1186/s13104-019-4447-1
Yaqo RT, Jalal SD, Ghafour KJ, Hassan HA, Hughson MD. Non-Hodgkin lymphoma in the Middle East is characterized by low incidence rates with advancing age. J Glob Oncol. 2019;5:1-10. doi: 10.1200/JGO.18.00233. DOI: https://doi.org/10.1200/JGO.18.00241
Balikó A, Szakács Z, Kajtár B, Ritter Z, Gyenesei A, Farkas N, et al. Clinicopathological analysis of diffuse large B-cell lymphoma using molecular biomarkers: a retrospective analysis from 7 Hungarian centers. Front Oncol. 2023;13:1224733. doi: 10.3389/fonc.2023.1224733. DOI: https://doi.org/10.3389/fonc.2023.1224733
Babu SM, Garg S, Kanakasetty GB, Kuntegowdanahalli LC, Dasappa L, Rao SA. Diffuse large B-cell lymphoma: a retrospective study from a regional care center in South India. Indian J Cancer. 2018;55(1):66-69. doi:10.4103/ijc.IJC_244_17. DOI: https://doi.org/10.4103/ijc.IJC_450_16
Okap IS, Tayel HY, Abd El AA, Nafea DA, Mashali NA. Correlation between germinal center differentiation and double/triple hit score in the classification of diffuse large B-cell non-Hodgkin lymphoma: a clinicopathological approach. Asian Pac J Cancer Care. 2023;8(1):77-82. doi: 10.31557/APJCC.2023.8.1.77. DOI: https://doi.org/10.31557/apjcc.2023.8.1.77-82
Ghongade P, Patil BU, Gupta A, Gangane NM. Clinicopathological presentation, prognosis, and overall survival of primary extranodal lymphomas. Med J DY Patil Vidyapeeth. 2025;18(1):71-79. doi: 10.4103/mjdrdypu.mjdrdypu_707_23. DOI: https://doi.org/10.4103/mjdrdypu.mjdrdypu_707_23
Lin W, Zuo W, Li Y, Yang Z, Chen J, Chen S, et al. Epidemiological characteristics and survival analysis of extranodal NK/T-cell lymphoma in China: a population-based study. Infect Agent Cancer. 2023;18(1):24. doi: 10.1186/s43556-023-00141-3. DOI: https://doi.org/10.1186/s43556-023-00141-3
Humam MA, Al-Nakhbi NA, Melkat AA, Almontaser TM, Binnabhan AS. Malignant lymphoma in Hadhramout sector, Yemen. J Curr Med Res Pract. 2016;1(2):6-11. doi: 10.4103/JCMRP.JCMRP_12_16. DOI: https://doi.org/10.4103/2357-0121.192538
Ortona E, Locatelli SL, Pagano MT, Ascione B, Careddu G, Dupuis ML, et al. The natural estrogen receptor beta agonist silibinin as a promising therapeutic tool in diffuse large B-cell lymphoma. Anticancer Res. 2022;42(2):767-779. doi: 10.21873/anticanres.15535. DOI: https://doi.org/10.21873/anticanres.15535
Radkiewicz C, Bruchfeld JB, Weibull CE, Jeppesen ML, Frederiksen H, Lambe M, et al. Sex differences in lymphoma incidence and mortality by subtype: a population-based study. Am J Hematol. 2023;98(1):23-30. doi: 10.1002/ajh.26744. DOI: https://doi.org/10.1002/ajh.26744
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. WHO classification of tumours of haematopoietic and lymphoid tissues. Revised 4th ed. Lyon: International Agency for Research on Cancer; 2017.
Khan M, Papier K, Pirie KL, Key TJ, Atkins J, Travis RC. Sex differences in cancer incidence: prospective analyses in the UK Biobank. Br J Cancer. 2025;132:1-1. doi: 10.1038/s41416-025-03123-5.
Schinasi L, Leon ME. Non-Hodgkin lymphoma and occupational exposure to agricultural pesticide chemical groups and active ingredients: a systematic review and meta-analysis. Int J Environ Res Public Health. 2014;11(4):4449. doi: 10.3390/ijerph110404449. DOI: https://doi.org/10.3390/ijerph110404449
Muhealdeen DN, Shwan A, Yaqo RT, Hassan HA, Muhammed BO, Ali RM, et al. Epstein-Barr virus and Burkitt’s lymphoma: associations in Iraqi Kurdistan and twenty-two countries assessed in the International Incidence of Childhood Cancer. Asian Pac J Cancer Care. 2021;6(1):37-44. doi: 10.31557/APJCC.2021.6.1.37. DOI: https://doi.org/10.1186/s13027-022-00452-0
Liu X, Kwon H, Li Z, Fu YX. Is CD47 an innate immune checkpoint for tumor evasion? J Hematol Oncol. 2017;10(1):12. doi: 10.1186/s13045-016-0381-z. DOI: https://doi.org/10.1186/s13045-016-0381-z
Cho J, Yoon SE, Kim SJ, Ko YH, Kim WS. CD47 overexpression is common in intestinal non-GCB type diffuse large B-cell lymphoma and associated with 18q21 gain. Blood Adv. 2022;6(24):6120-6130. doi: 10.1182/bloodadvances.2022008279. DOI: https://doi.org/10.1182/bloodadvances.2021006305
Gholiha AR, Hollander P, Löf L, Glimelius I, Hedström G, Molin D, et al. Checkpoint CD47 expression in classical Hodgkin lymphoma. Br J Haematol. 2022;197(5):580-589. doi: 10.1111/bjh.18137. DOI: https://doi.org/10.1111/bjh.18137
Testi AM, Al-Jadiry MF, Moleti ML, Uccini S, Al-Darraji AF, Al-Saeed RM, et al. Hodgkin lymphoma in children: a 16-year experience at the Children’s Welfare Teaching Hospital of Baghdad, Iraq. Mediterr J Hematol Infect Dis. 2024;16(1):e2024053. doi: 10.4084/mjhid.2024.053. DOI: https://doi.org/10.4084/MJHID.2024.053
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











