The Effect of Parents’ Perceived Stimulant Factors that Induce Asthma on the Quality of Life of their Children: A Cross-Sectional Study in Babylon, Iraq
DOI:
https://doi.org/10.54133/ajms.v7i1.1236Keywords:
Asthma, Child, Parents, Quality of LifeAbstract
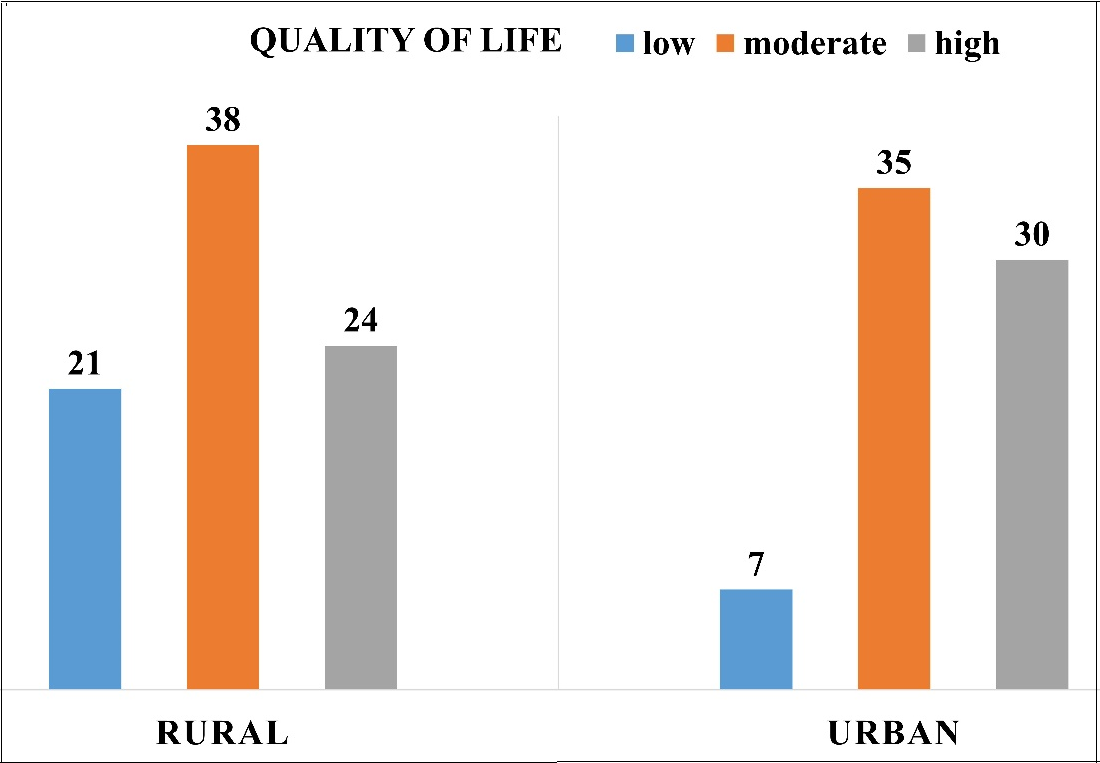
Background: Asthma is a chronic respiratory condition that causes wheezing, dyspnea, and coughing. Asthma symptoms can be increased by a variety of stimulants for each asthma subtype, affecting children's quality of life. Objectives: To assess the quality of life of children with asthma, identify parents' perceived stimulant factors that influence quality of life for asthmatic children, and determine relationships between quality of life, parents' perceived stimulant factors, and demographic data for asthmatic children and their parents. Methods: From October 4, 2023, to July 1, 2024, a descriptive study was done on parents of asthmatic children in Hillah City. A nonprobability purposive sample of 155 parents of school-aged asthmatic children was obtained using a specially designed method for the study. Results: The average age of the children was 8.8±2.1 years. The majority of the children were males from rural areas, and they were diagnosed between 4 and 5 years old. Parents identified weather as the most stimulating factor, followed by infections, irritants, exercise, emotions, obesity, allergens, and some drugs. The study found that the majority of asthmatic children had a decent quality of life, while parents with a a higher perception of stimulant variables have a lower quality of life. Conclusions: A high level of parents' perceived stimulant variables was negatively linked with quality of life among asthmatic children; additionally, residence, monthly income, and age of diagnosis were connected with quality of life.
Downloads
References
Carpaij OA, Burgess JK, Kerstjens HAM, Nawijn MC, Van Den Berge M. A review on the pathophysiology of asthma remission. Pharmacol Ther. 2019;201:8–24. doi: 10.1016/j.pharmthera.2019.05.002. DOI: https://doi.org/10.1016/j.pharmthera.2019.05.002
Barnes PJ. Asthma mechanisms. Medicine (Baltimore). 2016;44(5):265–270. doi: 10.1016/j.mpmed.2016.02.020. DOI: https://doi.org/10.1016/j.mpmed.2016.02.020
Nadhem R, Mohammed N, Hundhal A. Assessment of mother's knowledge concerning recurrent wheezy chest among children under age five years old at AL-Hilla hospitals/Iraq. J Pharm Sci Res. 2018;10(1):114-117.
Chen W, Marra CA, Lynd LD, FitzGerald JM, Zafari Z, Sadatsafavi M. The natural history of severe asthma and influences of early risk factors: a population-based cohort study. Thorax. 2016;71(3):267–75. doi: 10.1136/thoraxjnl-2015-207530. DOI: https://doi.org/10.1136/thoraxjnl-2015-207530
Wang R, Murray CS, Fowler SJ, Simpson A, Durrington HJ. Asthma diagnosis: into the fourth dimension. Thorax. 2021;76(6):624–631. doi: 10.1136/thoraxjnl-2020-216421. DOI: https://doi.org/10.1136/thoraxjnl-2020-216421
Landeo-Gutierrez J, Celedón JC. Chronic stress and asthma in adolescents. Ann Allergy Asthma Immunol. 2020;125(4):393-398. doi: 10.1016/j.anai.2020.07.001. DOI: https://doi.org/10.1016/j.anai.2020.07.001
Agrawal S, Iqbal S, Patel SJ, Freishtat R, Kochhar-Bryant C. Quality of life in at-risk school-aged children with asthma. J Asthma. 2021;58(12):1680-1688. doi: 10.1080/02770903.2020.1825732. DOI: https://doi.org/10.1080/02770903.2020.1825732
Alsayed B, Alatawi A, Alatawi OM, Alatawi RH, Alfuhaymani AM, Aljohani JK. Association of asthma control with caregivers’ knowledge and practices for children with asthma in the Tabuk region of Saudi Arabia: A cross-sectional study. Cureus. 2023. doi: 10.7759/cureus.35162. DOI: https://doi.org/10.7759/cureus.35162
Pars H, Soyer Ö, Şekerel BE. The experiences, perceptions and challenges of mothers managing asthma in their children: a qualitative study. Turk J Pediatr. 2020;62(5):734-745. doi: 10.24953/turkjped.2020.05.004. DOI: https://doi.org/10.24953/turkjped.2020.05.004
Hashim HME, Ismail AM, Abd Elraouf MS, Saber MMA, Hassan HAA. Knowledge and self-care management practice among asthmatic children (6-12 years): an educational intervention study. Egypt J Hosp Med. 2022;88(1):2599-2605. doi: 10.21608/ejhm.2022.240871. DOI: https://doi.org/10.21608/ejhm.2022.240871
Mazi A, Madani F, Alsulami E, Almutari A, Alamri R, Jahhaf J, et al. Uncontrolled asthma among children and its association with parents’ asthma knowledge and other socioeconomic and environmental factors. Cureus. 2023;15(2). doi: 10.7759/cureus.35240. DOI: https://doi.org/10.7759/cureus.35240
Al-Sammak NI, Jamel SH, Ibrahim AT. Asthma knowledge and behaviours among parents of asthmatic children attending paediatric hospitals in Mosul City. Medico-Legal Update. 2020;20(4):429-434. doi: 10.37506/mlu.v20i4.1940. DOI: https://doi.org/10.37506/mlu.v20i4.1940
Owora AH, Zhang Y. Childhood wheeze trajectory-specific risk factors: a systematic review and meta-analysis. Pediatr Allergy Immunol. 2021;32(1):34-50. doi: 10.1111/pai.13313. DOI: https://doi.org/10.1111/pai.13313
Chipps BE, Soong W, Panettieri Jr RA, Carr W, Gandhi H, Zhou W, et al. Number of patient-reported asthma triggers predicts uncontrolled disease among specialist-treated patients with severe asthma. Ann Allergy Asthma Immunol. 2023;130(6):784-790. doi: 10.1016/j.anai.2023.03.001. DOI: https://doi.org/10.1016/j.anai.2023.03.001
Mamluk MS, Karadakhy KA. Aggravating factors of asthma among patients visited respiratory center at Shar Hospital outpatient in Sulaymaniyah-Kurdistan-Iraq. Adv Med J. 2024;9(2):19-26. doi: 10.56056/amj.2024.253 DOI: https://doi.org/10.56056/amj.2024.253
Bianchi-Hayes JM, Cataldo R, Schoenfeld ER, Hou W, Pati S. Caregivers’ perceptions of the relationship among weight, health status, and asthma in their children. J Child Health Care. 2020;25(4):647-658. doi: 10.1177/1367493520985719. DOI: https://doi.org/10.1177/1367493520985719
Kamath SP, Shrishakumar S, Jain A, Ramakrishna A, Baliga SB. Risk and triggering factors associated with bronchial asthma among school-going children in an urban city of coastal Karnataka. J Nepal Paediatr Soc. 2017;37(1):64-70. doi: 10.3126/jnps.v37i1.16634. DOI: https://doi.org/10.3126/jnps.v37i1.16634
Akhiwu HO, Nantok D, Oguche S. Assessment of the health-related quality of life in children with asthma in a tertiary hospital in North Central, Nigeria. Pan Afr Med J. 2022;41:144. doi: 10.11604/pamj.2022.41.58.30171. DOI: https://doi.org/10.11604/pamj.2022.41.58.30171
Plaza-González S, Zabala-Baños MDC, Astasio-Picado Á, Jurado-Palomo J. Psychological and sociocultural determinants in childhood asthma disease: impact on quality of life. Int J Environ Res Public Health. 2022;19(5):2652. doi: 10.3390%2Fijerph19052652. DOI: https://doi.org/10.3390/ijerph19052652
Toyran M, Yagmur IT, Guvenir H, Haci IA, Bahceci S, Batmaz SB, et al. Asthma control affects school absence, achievement and quality of school life: a multicenter study. Allergol Immunopathol (Madr). 2020;48(6):545-552. doi: 10.1016/j.aller.2020.05.005. DOI: https://doi.org/10.1016/j.aller.2020.05.005
Kansen HM, Le TM, Meijer Y, Uiterwaal CS, Knulst AC, van Der Ent CK, et al. Perceived triggers of asthma impair quality of life in children with asthma. Clin Exp Allergy. 2019;49(7):980-989. doi.org/10.1111%2Fcea.13407. DOI: https://doi.org/10.1111/cea.13407
Janssens T, Harver A. Effects of symptom perception interventions on trigger identification and quality of life in children with asthma. Pulm Med. 2015;2015:825137. doi: 10.1155/2015/825137. DOI: https://doi.org/10.1155/2015/825137
Abegaz TM, Shegena EA, Gessie NF, Gebreyohannes EA, Seid MA. Barriers to and competency with the use of metered dose inhaler and its impact on disease control among adult asthmatic patients in Ethiopia. BMC Pulm Med. 2020;20(1):54. doi: 10.1186/s12890-020-1081-6. DOI: https://doi.org/10.1186/s12890-020-1081-6
Shi M, Liang L, Wang Y, Yu Y. Risk factors associated with health-related quality of life in pediatric asthma. Sci Prog. 2021;104(2):00368504211013657. doi: 10.1177%2F00368504211013657. DOI: https://doi.org/10.1177/00368504211013657
Čibirkaitė M, Bubnaitienė V, Hansted E, Gurskis V, Vaidelienė L. Quality-of-life assessment in children with mild to moderate bronchial asthma. Medicina (Kaunas). 2021;57(1):10. doi: 10.3390/medicina60050771. DOI: https://doi.org/10.3390/medicina60050771
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











