Viral Etiology and its Association with Demographics and Clinical Characteristics in Children Hospitalized for Watery Diarrhea
DOI:
https://doi.org/10.54133/ajms.v8i1.1700Keywords:
Adenovirus, Children, Gastroenteritis, Rotavirus, Watery diarrheaAbstract
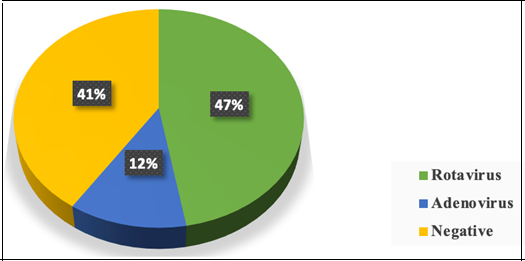
Background: Acute infectious gastroenteritis (AG) stands for one of the commonest causes of death in children under 5 years of age. Objective: To assess the prevalence of viral etiology in children hospitalized for watery diarrhea and identify the relation between patients’ characteristics and the underlying viral etiology of AG. Methods: A cross-sectional study included children hospitalized with AG who presented with watery diarrhea. Three sets of data were collected: the sociodemographic characteristics (age, gender, residence, type of feeding, method of sterilization, number of family members, and socioeconomic status), the clinical characteristics (duration of illness, frequency of diarrhea per day, presence of vomiting, degree of dehydration, fever, and napkin rash), and the laboratory result (white blood cell count, C-reactive protein, pus on general stool exam, and the type of viral etiology detected in the stool by immunoassay). Results: A total of 216 children aged less than 5 years were included, with 170(78.7%) who were less than 1 year of age. Less than two-thirds of the patients (59%) had identified viral etiology, in which 102 children (47%) had rotavirus in their stool and 26(12%) adenoviruses were detected. Four sociodemographic factors were significantly related to the viral etiology: age less than 1 year, male sex in adenovirus and female in rotavirus, formula feeding, and socioeconomic status. Conclusions: The study highlights an increasing frequency of viral detection in children hospitalized with watery diarrhea, with rotavirus remaining the most identified pathogen, followed by adenovirus.
Downloads
References
Troeger C, Blacker BF, Khalil IA, Rao PC, Cao S, Zimsen SR, et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect Dis. 2018;18. doi: 10.1016/S1473-3099(18)30362-1. DOI: https://doi.org/10.1016/S1473-3099(18)30362-1
Glass RI, Parashar UD, Bresee JS, Turcios R, Fischer TK, Widdowson MA, et al. Rotavirus vaccines: current prospects and future challenges. Lancet. 2006;368. doi: 10.1016/S0140-6736(06)68815-6. DOI: https://doi.org/10.1016/S0140-6736(06)68815-6
Abdulazeez MS, Al-Shuwaikh AM, Latif II. Detection and comparison of Sapovirus, rotavirus and norovirus among infants and young children with acute gastroenteritis. Ann Trop Med Public Health. 2020;23. doi: 10.36295/ASRO.2020.231439. DOI: https://doi.org/10.36295/ASRO.2020.231439
Zhou HL, Bessey T, Wang SM, Mo ZJ, Barclay L, Wang JX, et al. Burden and etiology of moderate and severe diarrhea in children less than 5 years of age living in north and south of China: Prospective, population-based surveillance. Gut Pathog. 2021;13. doi: 10.1186/s13099-021-00428-2 . DOI: https://doi.org/10.1186/s13099-021-00428-2
Hassan F, Kanwar N, Harrison CJ, Halasa NB, Chappell JD, Englund JA, et al. Viral etiology of acute gastroenteritis in <2-Year-Old US children in the post-rotavirus vaccine era. J Pediatric Infect Dis Soc. 2019;8. doi: 10.1093/jpids/piy077. DOI: https://doi.org/10.1093/jpids/piy077
Mohamed NS, Hameed MF, Al-Rubai HK. Detection of norovirus and rotavirus in children under five years during winter 2012-2013 in Mosul province. J Al-Nahrain Univ Sci. 2016;19:101–107. doi: 10.22401/JNUS.19.3.13. DOI: https://doi.org/10.22401/JNUS.19.3.13
Rivadulla E, Romalde JL. A Comprehensive review on human aichi virus. Virol Sin. 2020;35. doi: 10.1007/s12250-020-00222-5. DOI: https://doi.org/10.1007/s12250-020-00222-5
Mohammad YM, Al-Shuwaikh AM, Al-Hamdani HT. Bocavirus and rotavirus co-infection in children with acute gastroenteritis and associated risk factors. Diyala J Med. 2023;25. doi: 10.26505/djm.v25i1.1031. DOI: https://doi.org/10.26505/DJM.25017430323
Thwiny HT, Alsalih NJ, Saeed ZF, Al-Yasari AMR, Al-Saadawe MAA, Alsaadawi MAE. Prevalence and seasonal pattern of enteric viruses among hospitalized children with acute gastroenteritis in Samawah, Iraq. J Med Life. 2022;15. doi: 10.25122/jml-2021-0158. DOI: https://doi.org/10.25122/jml-2021-0158
Dennehy PH, Cortese MM, Bégué RE, Jaeger JL, Roberts NE, Zhang R, et al. A case-control study to determine risk factors for hospitalization for rotavirus gastroenteritis in U.S. children. Pediatr Infect Dis J. 2006;25. doi: 10.1097/01.inf.0000243777.01375.5b. DOI: https://doi.org/10.1097/01.inf.0000243777.01375.5b
Kotloff KL, Nataro JP, Blackwelder WC, Nasrin D, Farag TH, Panchalingam S, et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): A prospective, case-control study. Lancet. 2013;382. doi: 10.1016/S0140-6736(13)60844-2. DOI: https://doi.org/10.1016/S0140-6736(13)60844-2
Brander RL, Pavlinac PB, Walson JL, John-Stewart GC, Weaver MR, Faruque ASG, et al. Determinants of linear growth faltering among children with moderate-to-severe diarrhea in the Global Enteric Multicenter Study. BMC Med. 2019;17. doi: 10.1186/s12916-019-1441-3. DOI: https://doi.org/10.1186/s12916-019-1441-3
Posovszky C, Buderus S, Claben M, Hauer A, Lawrenz B, Koletzko S, et al. Recommendations for action according to the “S2k guidelines on acute infectious gastroenteritis in infancy, childhood and adolescence.” Monatsschr Kinderheilkd. 2020;168. doi: 10.1007/s00112-019-00813-x. DOI: https://doi.org/10.1007/s00112-019-00813-x
Chitambar S, Gopalkrishna V, Chhabra P, Patil P, Verma H, Lahon A, et al. Diversity in the enteric viruses detected in outbreaks of gastroenteritis from Mumbai, Western India. Int J Environ Res Public Health. 2012;9. doi: 10.3390/ijerph9030895. DOI: https://doi.org/10.3390/ijerph9030895
Ayukekbong J, Lindh M, Nenonen N, Tah F, Nkuo-Akenji T, Bergström T. Enteric viruses in healthy children in Cameroon: Viral load and genotyping of norovirus strains. J Med Virol. 2011;83. doi: 10.1002/jmv.22243. DOI: https://doi.org/10.1002/jmv.22243
Mohtar J, Mallah H, Mardirossian JM, El-Bikai R, Jisr T El, Soussi S, et al. Enhancing enteric pathogen detection: implementation and impact of multiplex PCR for improved diagnosis and surveillance. BMC Infect Dis. 2024;24. doi: 10.1186/s12879-024-09047-z. DOI: https://doi.org/10.1186/s12879-024-09047-z
Babaei A, Rafiee N, Taheri B, Sohrabi H, Mokhtarzadeh A. Recent advances in early diagnosis of viruses associated with gastroenteritis by biosensors. Biosensors (Basel). 2022;12. doi: 10.3390/bios12070499. DOI: https://doi.org/10.3390/bios12070499
Calderaro A, Buttrini M, Montecchini S, Rossi S, Farina B, Arcangeletti MC, et al. Prevalence of intestinal parasitosis in a non-endemic setting during a 10-year period (2011–2020): A Focus on Dientamoeba fragilis. Microorganisms. 2022;10. doi: 10.3390/microorganisms10020426. DOI: https://doi.org/10.3390/microorganisms10020426
Arvind N, Sushma M, Krishnappa J. Prevalence of rotavirus and adenovirus in the childhood gastroenteritis in a tertiary care teaching hospital. J Pure Appl Microbiol. 2019;13. doi: 10.22207/JPAM.13.2.38. DOI: https://doi.org/10.22207/JPAM.13.2.38
Moe CL, Allen JR, Monroe SS, Gary HE, Humphrey CD, Herrmann JE, et al. Detection of astrovirus in pediatric stool samples by immunoassay and RNA probe. J Clin Microbiol. 1991;29. doi: 10.1128/jcm.29.11.2390-2395.1991. DOI: https://doi.org/10.1128/jcm.29.11.2390-2395.1991
Shet N, Gupta V, Wan D. Stool tools: PCR detection of astrovirus and sapovirus. Am J Gastroenterol. 2017;112. doi: 10.14309/00000434-201710001-02397. DOI: https://doi.org/10.14309/00000434-201710001-02397
Hyun J, Ko DH, Lee SK, Kim HS, Kim JS, Song W, et al. Evaluation of a new multiplex real-time PCR assay for detecting gastroenteritis-causing viruses in stool samples. Ann Lab Med. 2018;38. doi: 10.3343/alm.2018.38.3.220. DOI: https://doi.org/10.3343/alm.2018.38.3.220
Nasser AT, Hasan AS, Saleh AK, Saleh MK. Immunological and molecular detection of rotavirus genotype in children with gastroenteritis in Diyala-Iraq. GSC Adv Res Rev. 2021;06. doi: 10.30574/gscarr.2021.6.3.0056. DOI: https://doi.org/10.30574/gscarr.2021.6.3.0056
Sarhan AT, Alkhazraji EK, Al-Meamar TS. Prevalence of pediatric gastroenteritis disease in Al-Diwaniyah governorate-Iraq. Indian J Forensic Med Toxicol. 2021;15. doi: 10.37506/ijfmt.v15i4.16678. DOI: https://doi.org/10.37506/ijfmt.v15i4.16678
Al-Tabtabai AMH, Al-Rubaey NKF, Al-Zamily KY. Detection of rotavirus, norovirus and astrovirus among children with acute gastroenteritis in Babylon governorate, Iraq. Biochem Cell Arch. 2020;20.
Abdulridha AS. Study the effects of age and gender of children on rotavirus infection in Baghdad, Iraq. Res J Pharm Biol Chem Sci. 2016;7.
Al-Janabi MK, Al-Ahmer SD, Al-Hamdani FG. Study of the association of rotavirus and astrovirus in children infected with acute gastroenteritis in Baghdad city. Plant Arch. 2020;20.
Fenjan M, Jarullah B. Molecular identification and phylogenetic analysis of rotavirus in children suffered from diarrhea under five years old In Thi-Qar province, Iraq. J Coll Edu Pure Sci. 2019;9. doi: 10.32792/utq.jceps.09.01.09. DOI: https://doi.org/10.32792/utq.jceps.09.01.09
Habash SH, Issa Habeeb S. Rotavirus diarrhea in children under five in Basrah: Hospital based study. Pediatr Infect Dis. 2018;03. doi: 10.21767/2573-0282.100062. DOI: https://doi.org/10.21767/2573-0282.100062
Akram NN, Sadoon ST, Jaafar MM, Nori W. Factors affecting parental refusal of lumbar puncture in Iraqi children in COVID-19 era: a cross-sectional study. J Pak Med Assoc. 2024;74:S219–222. doi: 10.47391/JPMA-BAGH-16-49. DOI: https://doi.org/10.47391/JPMA-BAGH-16-49
Barros LL, Barros LL, do Carmo RF, Santos MB, da Costa Armstrong A, de Vasconcelos RA, et al. Change in rotavirus vaccine coverage in Brazil from before (2015–2019) through the COVID-19 pandemic period (2020–2021). Viruses. 2023;15. doi: 10.3390/v15020292. DOI: https://doi.org/10.3390/v15020292
Akram NN, Nori W, Al Qaissi KW, Abdulrahman Hadi BA. Multi-systemic inflammatory syndrome in childhood (MIS-C): A review article. J Pak Med Assoc. 2021;71.
Scarano SM, Lo Vecchio A. How to make up for rotavirus vaccination missed during the COVID-19 pandemic? JAMA Pediatr. 2022;176. doi: 10.1001/jamapediatrics.2021.6022. DOI: https://doi.org/10.1001/jamapediatrics.2021.6022
Desilva MB, Weintraub E, Kharbanda EO. How to make up for rotavirus vaccination missed during the COVID-19 pandemic? Reply. JAMA Pediatr. 2022;176. doi: 10.1001/jamapediatrics.2021.6019. DOI: https://doi.org/10.1001/jamapediatrics.2021.6019
Sciarra F, Campolo F, Franceschini E, Carlomagno F, Venneri MA. Gender-specific impact of sex hormones on the immune system. Int J Mol Sci. 2023;24. doi: 10.3390/ijms24076302. DOI: https://doi.org/10.3390/ijms24076302
Tahmasebi R, Luchs A, Tardy K, Hefford PM, Tinker RJ, Eilami O, et al. Viral gastroenteritis in Tocantins, Brazil: Characterizing the diversity of human adenovirus F through next-generation sequencing and bioinformatics. J Gen Virol. 2021;101. doi: 10.1099/jgv.0.001500. DOI: https://doi.org/10.1099/jgv.0.001500
Kumthip K, Khamrin P, Ushijima H, Maneekarn N. Enteric and non-enteric adenoviruses associated with acute gastroenteritis in pediatric patients in Thailand, 2011 to 2017. PLoS One. 2019;14. doi: 10.1371/journal.pone.0220263. DOI: https://doi.org/10.1371/journal.pone.0220263
Latifi T, Kachooei A, Jalilvand S, Zafarian S, Roohvand F, Shoja Z. Correlates of immune protection against human rotaviruses: natural infection and vaccination. Arch Virol. 2024;169. doi: 10.1007/s00705-024-05975-y. DOI: https://doi.org/10.1007/s00705-024-05975-y
Mccormick BJJ, Richard SA, Murray-Kolb LE, Kang G, Lima AAM, Mduma E, et al. Full breastfeeding protection against common enteric bacteria and viruses: Results from the MAL-ED cohort study. Am J Clin Nutr. 2022;115. doi: 10.1093/ajcn/nqab391. DOI: https://doi.org/10.1093/ajcn/nqab391
Mathur KS, Dwivedi V. Optimal control of rotavirus infection in breastfed and non-breastfed children. Result Control Optimiz. 2024;16:100452. doi: 10.1016/J.RICO.2024.100452. DOI: https://doi.org/10.1016/j.rico.2024.100452
Nori W, Akram NN, Al-Kaabi MM. Probiotics in women and pediatrics health: A narrative review. Al-Anbar Med J. 2023;19. doi: 10.33091/amj.2023.138442.1021. DOI: https://doi.org/10.33091/amj.2023.138442.1021
Ma J, Li Z, Zhang W, Zhang C, Zhang Y, Mei H, et al. Comparison of gut microbiota in exclusively breast-fed and formula-fed babies: a study of 91 term infants. Sci Rep. 2020;10. doi: 10.1038/s41598-020-72635-x. DOI: https://doi.org/10.1038/s41598-020-72635-x
Uhnoo I. Clinical features of acute gastroenteritis associated with rotavirus, enteric adenovirus, and bacteria. Pediatr Infect Dis J. 1987;6. doi: 10.1097/00006454-198702000-00027. DOI: https://doi.org/10.1097/00006454-198702000-00027
Zaraket R, Salami A, Bahmad M, El Roz A, Khalaf B, Ghssein G, et al. Prevalence, risk factors, and clinical characteristics of rotavirus and adenovirus among Lebanese hospitalized children with acute gastroenteritis. Heliyon. 2020;6. doi: 10.1016/j.heliyon.2020.e04248. DOI: https://doi.org/10.1016/j.heliyon.2020.e04248
Joshi MS, Sukirti V, Chavan NA, Walimbe AM, Potdar VA, Vipat VC, et al. Enteric and non-enteric adenoviruses in children with acute gastroenteritis in Western India. Infect Genet Evol. 2023;112. doi: 10.1016/j.meegid.2023.105454. DOI: https://doi.org/10.1016/j.meegid.2023.105454
Akram NN, Jaafar MM, Abdulqader SK, Nori W, Kassim MAK, Pantazi AC. Clinical characteristics and therapeutic management of osteogenesis imperfecta in Iraqi children. Al-Rafidain J Med Sci. 2023;5:S189-194. doi: 10.54133/ajms.v5i1s.416. DOI: https://doi.org/10.54133/ajms.v5i1S.416
Abdul AL-Kader RA, Hassan A. Rota virus diarrhea in children under five admitted to Basrah general hospital. Med J Basrah Univ. 2016;34:107–114. doi: 10.33762/mjbu.2016.117213. DOI: https://doi.org/10.33762/mjbu.2016.117213
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











