Understanding Attention Deficit Hyperactivity Disorder: Prevalence, Etiology, Diagnosis, and Therapeutic Approaches
DOI:
https://doi.org/10.54133/ajms.v7i1.756Keywords:
ADHD, Diagnosis, Etiology, Prevalence, Stimulants and non-stimulantAbstract
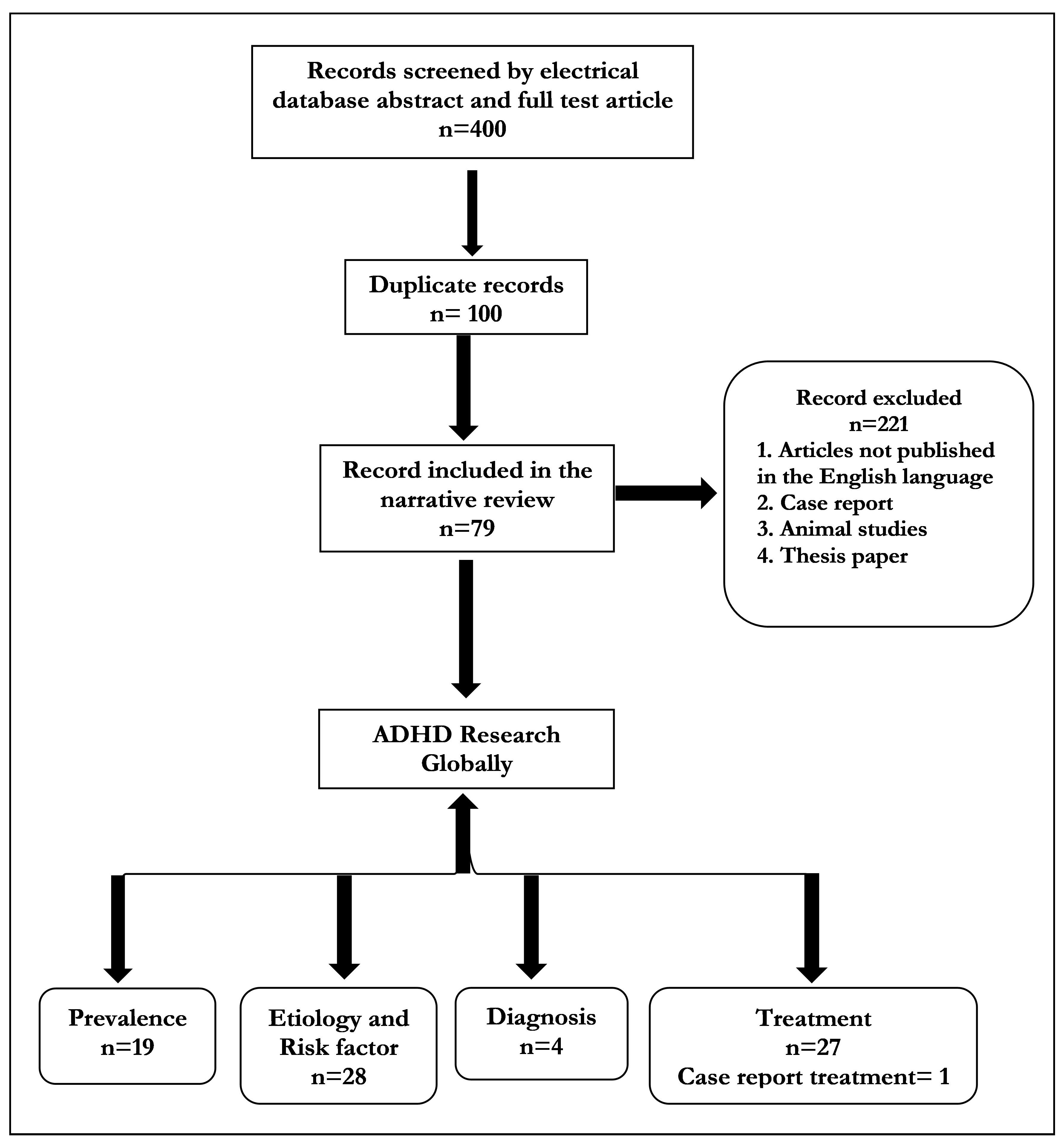
Background: Attention deficit hyperactivity disorder (ADHD) is classified using neoclassical systems such as the Diagnostic Statistical Manual of Mental Disorders-5 and the International Classification of Disease-10. There is significant evidence that pharmaceutical treatment, particularly stimulants, can reduce symptoms in the short term. Objective: To explore the comprehensive landscape of childhood to adulthood ADHD within the literature, which involves delving into its prevalence, etiology, risk factors, diagnosis, and treatment modalities. Methods: A literature search was conducted across articles published in English between 2011 and 2023; the literature extensively explored the prevalence, etiology, risk factors and diagnosis of the subject, with limited attention given to treatment between 2003 and 2023, utilizing electronic search engines such as Google Scholar, PubMed, IndMED, and MedIND, Scopus, and Web of Science. The search terms included "ADHD," "Attention Deficit and Hyperactivity Disorder," "Hyperactivity," "Child Psychiatry," "Hyperkinetic Disorder," "Attention Deficit Disorder," and "Worldwide.” Results: Out of the 400 papers evaluated, only 52 met the criteria encompassing prevalence, etiology, diagnosis, and treatment. Conclusions: ADHD is a prevalent neurodevelopmental disorder impacting individuals from childhood to adulthood, with varying prevalence rates globally. Methodological differences influence prevalence estimates, highlighting the need for standardized study designs. Both genetic and environmental factors contribute to its development. Management typically involves a combination of psychotherapy, lifestyle adjustments, and medication. However, refined diagnostic criteria and tailored treatment guidelines for children and adults are necessary. Continuous evaluation of interventions is crucial for optimizing care and enhancing the well-being of individuals with ADHD.
Downloads
References
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Diagnostic and Statistical Manual of Mental Disorders 2013. doi: 10.1176/APPI.BOOKS.9780890425596. DOI: https://doi.org/10.1176/appi.books.9780890425596
Berger I. Diagnosis of attention deficit hyperactivity disorder: much ado about something. Isr Med Assoc J. 2011;13(9):571-574. PMID: 21991721.
Drechsler R, Brem S, Brandeis D, Grünblatt E, Berger G, Walitza S. ADHD: Current concepts and treatments in children and adolescents. Neuropediatrics. 2020;51:315. doi: 10.1055/S-0040-1701658. DOI: https://doi.org/10.1055/s-0040-1701658
Dvorsky MR, Langberg JM. A review of factors that promote resilience in youth with ADHD and ADHD symptoms. Clin Child Fam Psychol Rev. 2016;19:368–3691. doi: 10.1007/S10567-016-0216-Z. DOI: https://doi.org/10.1007/s10567-016-0216-z
Goldstein S, Ellison AT, (eds.), Clinicians’ Guide to Adult ADHD: Assessment and Intervention, (6th Ed.), Academic Press; 2002. P. 301.
Faraone SV, Banaschewski T, Coghill D, Zheng Y, Biederman J, Bellgrove MA, et al. The World federation of ADHD international consensus statement: 2008 Evidence-based conclusions about the disorder. Neurosci Biobehav Rev. 2021;128:789–818. doi: 10.1016/j.neubiorev.2021.01.022. DOI: https://doi.org/10.1016/j.neubiorev.2021.01.022
Foreman DM. Attention deficit hyperactivity disorder: legal and ethical aspects. Arch Dis Child. 2006;91:192–194. doi: 10.1136/adc.2004.064576. DOI: https://doi.org/10.1136/adc.2004.064576
Wilens TE, Spencer TJ. Understanding attention-deficit/hyperactivity disorder from childhood to adulthood. Postgrad Med. 2010;122:97. doi: 10.3810/PGM.2010.09.2206. DOI: https://doi.org/10.3810/pgm.2010.09.2206
Thomas R, Sanders S, Doust J, Beller E, Glasziou P. Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics. 2015;135:e994–1001. doi: 10.1542/PEDS.2014-3482. DOI: https://doi.org/10.1542/peds.2014-3482
Song P, Zha M, Yang Q, Zhang Y, Li X, Rudan I. The prevalence of adult attention-deficit hyperactivity disorder: A global systematic review and meta-analysis. J Glob Health. 2021;11:1–9. doi: 10.7189/JOGH.11.04009. DOI: https://doi.org/10.7189/jogh.11.04009
Ayano G, Demelash S, Gizachew Y, Tsegay L, Alati R. The global prevalence of attention deficit hyperactivity disorder in children and adolescents: An umbrella review of meta-analyses. J Affect Disord. 2023;339:860–866. doi: 10.1016/J.JAD.2023.07.071. DOI: https://doi.org/10.1016/j.jad.2023.07.071
Ayano G, Yohannes K, Abraha M. Epidemiology of attention-deficit/hyperactivity disorder (ADHD) in children and adolescents in Africa: a systematic review and meta-analysis. Ann Gen Psychiatry. 2020;19. doi: 10.1186/S12991-020-00271-W. DOI: https://doi.org/10.1186/s12991-020-00271-w
Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatr. 2015;56:345–365. doi: 10.1111/JCPP.12381. DOI: https://doi.org/10.1111/jcpp.12381
Cénat JM, Kokou-Kpolou CK, Blais-Rochette C, Morse C, Vandette MP, Dalexis RD, et al. Prevalence of ADHD among black youth compared to white, Latino and Asian youth: A meta-analysis. J Clin Child Adolesc Psychol. 2022. doi: 10.1080/15374416.2022.2051524. DOI: https://doi.org/10.1080/15374416.2022.2051524
Vasileva M, Graf RK, Reinelt T, Petermann U, Petermann F. Research review: A meta-analysis of the international prevalence and comorbidity of mental disorders in children between 1 and 7 years. J Child Psychol Psychiatr. 2021;62:372–381. doi: 10.1111/JCPP.13261. DOI: https://doi.org/10.1111/jcpp.13261
Wang T, Liu K, Li Z, Xu Y, Liu Y, Shi W, et al. Prevalence of attention deficit/hyperactivity disorder among children and adolescents in China: a systematic review and meta-analysis. BMC Psychiatry. 2017;17. doi; 10.1186/S12888-016-1187-9. DOI: https://doi.org/10.1186/s12888-016-1187-9
Yadegari N, Sayehmiri K, Azodi MZ, Sayehmiri F, Modara F. The prevalence of attention deficient hyperactivity disorder among Iranian children: A meta-analysis. Iranian J Psychiatr Behav Sci. 2018;12:8990. doi: 10.5812/IJPBS.8990. DOI: https://doi.org/10.5812/ijpbs.8990
Ganesh S, Kandasamy A, Sahayaraj US, Benegal V. Adult attention deficit hyperactivity disorder in patients with substance use disorders: A study from southern India. Indian J Psychol Med. 2017;39:59. doi: 10.4103/0253-7176.198945. DOI: https://doi.org/10.4103/0253-7176.198945
Jaisoorya TS, Gowda GS, Nair BS, Menon PG, Rani A, Radhakrishnan KS, et al. Correlates of high-risk and low-risk alcohol use among college students in Kerala, India. J Psychoactive Drugs. 2018;50:54–61. doi; 10.1080/02791072.2017.1370748. DOI: https://doi.org/10.1080/02791072.2017.1370748
Lohit S, Babu G, Sharma S, Rao S, Sachin B, Matkar A. Prevalence of adult ADHD co-morbidity in alcohol use disorders in a general hospital setup. Indian J Psychol Med. 2019;41:523. doi: 10.4103/IJPSYM.IJPSYM_464_18. DOI: https://doi.org/10.4103/IJPSYM.IJPSYM_464_18
Gupta S, Bhatia G, Sarkar S, Chatterjee B, Balhara YPS, Dhawan A. Adult attention-deficit hyperactivity disorders and its correlates in patients with opioid dependence: An exploratory study. Indian J Psychiatr. 2020;62:501–508. doi: 10.4103/PSYCHIATRY.INDIANJPSYCHIATRY_705_19. DOI: https://doi.org/10.4103/psychiatry.IndianJPsychiatry_705_19
Ganesan SP, Lokesh Kumar K. Chilukuri H. Relation of substance use to attention deficit hyperactivity disorder among undergraduate students: a cross-sectional survey. Int J Indian Psychol. 2021;9(1):1090-1099. doi: 10.25215/0901.114.
Dhagudu N, Reddy M, Kumar O. Prevalence and profile of adult attention deficit hyperactive disorder in alcohol use disorder: An explorative study. Telangana J Psychiatr. 2021;7:94. doi: 10.4103/TJP.TJP_43_21. DOI: https://doi.org/10.4103/tjp.tjp_43_21
Kumar S, Venkatakrishna S, Kota S. Adult attention deficit hyperactivity disorder and Its correlates with the presence and severity of early-onset alcohol dependence: An estimate from a tertiary care center. Indian J Private Psychiatr. 2021. doi: 10.5005/jp-journals-10067-0075. DOI: https://doi.org/10.5005/jp-journals-10067-0075
Samal B, Senjam G, Ravan JR, Ningombam HS, Das RC, Das SK. Prevalence of adult ADHD in patients with substance use disorder in North East India. Ind Psychiatr J. 2022;31:214. doi: 10.4103/IPJ.IPJ_250_21. DOI: https://doi.org/10.4103/ipj.ipj_250_21
Rohner H, Gaspar N, Philipsen A, Schulze M. Prevalence of attention deficit hyperactivity disorder (ADHD) among substance use disorder (SUD) populations: Meta-analysis. Int J Environ Res Public Health. 2023;20:1275. doi: 10.3390/IJERPH20021275. DOI: https://doi.org/10.3390/ijerph20021275
van Emmerik-van Oortmerssen K, van de Glind G, van den Brink W, Smit F, Crunelle CL, Swets M, et al. Prevalence of attention-deficit hyperactivity disorder in substance use disorder patients: A meta-analysis and meta-regression analysis. Drug Alcohol Depend. 2012;122:11–19. doi: 10.1016/j.drugalcdep.2011.12.007. DOI: https://doi.org/10.1016/j.drugalcdep.2011.12.007
Wilens TE, Morrison NR. Substance-use disorders in adolescents and adults with ADHD: focus on treatment. Neuropsychiatry. 2012;2:301. doi: 10.2217/NPY.12.39. DOI: https://doi.org/10.2217/npy.12.39
van de Glind G, Konstenius M, Koeter MWJ, van Emmerik-van Oortmerssen K, Carpentier PJ, Kaye S, et al. Variability in the prevalence of adult ADHD in treatment seeking substance use disorder patients: Results from an international multi-center study exploring DSM-IV and DSM-5 criteria. Drug Alcohol Depend. 2014;134:158. doi: 10.1016/j.drugalcdep.2013.09.026. DOI: https://doi.org/10.1016/j.drugalcdep.2013.09.026
Srichawla BS, Telles CC, Schweitzer M, Darwish B. Attention deficit hyperactivity disorder and substance use disorder: A narrative review. Cureus. 2022;14. doi: 10.7759/cureus.24068. DOI: https://doi.org/10.7759/cureus.24068
Leppert B, Havdahl A, Riglin L, Jones HJ, Zheng J, Davey Smith G, et al. Association of maternal neurodevelopmental risk alleles with early-life exposures. JAMA Psychiatry. 2019;76:834–842. doi: 10.1001/jamapsychiatry.2019.0774. DOI: https://doi.org/10.1001/jamapsychiatry.2019.0774
Thapar A, Rutter M. Do natural experiments have an important future in the study of mental disorders? Psychol Med. 2019;49:1079–1088. doi: 10.1017/S0033291718003896. DOI: https://doi.org/10.1017/S0033291718003896
Rivollier F, Krebs MO, Kebir O. Perinatal exposure to environmental endocrine disruptors in the emergence of neurodevelopmental psychiatric diseases: A systematic review. Int J Environ Res Public Health. 2019;16. doi: 10.3390/ijerph16081318. DOI: https://doi.org/10.3390/ijerph16081318
Myhre O, Låg M, Villanger GD, Oftedal B, Øvrevik J, Holme JA, et al. Early life exposure to air pollution particulate matter (PM) as risk factor for attention deficit/hyperactivity disorder (ADHD): Need for novel strategies for mechanisms and causalities. Toxicol Appl Pharmacol. 2018;354:196–214. doi: 10.1016/j.taap.2018.03.015. DOI: https://doi.org/10.1016/j.taap.2018.03.015
Nigg JT, Elmore AL, Natarajan N, Friderici KH, Nikolas MA. Variation in an iron metabolism gene moderates the association between blood lead levels and attention-deficit/hyperactivity disorder in children. Psychol Sci. 2016;27:257–269. doi: 10.1177/0956797615618365. DOI: https://doi.org/10.1177/0956797615618365
Goodlad JK, Marcus DK, Fulton JJ. Lead and attention-deficit/hyperactivity disorder (ADHD) symptoms: A meta-analysis. Clin Psychol Rev. 2013;33:417–425. doi: 10.1016/j.cpr.2013.01.009. DOI: https://doi.org/10.1016/j.cpr.2013.01.009
Björkenstam E, Björkenstam C, Jablonska B, Kosidou K. Cumulative exposure to childhood adversity, and treated attention deficit/hyperactivity disorder: a cohort study of 543 650 adolescents and young adults in Sweden. Psychol Med. 2018;48:498–507. doi: 10.1017/S0033291717001933. DOI: https://doi.org/10.1017/S0033291717001933
Serati M, Barkin JL, Orsenigo G, Altamura AC, Buoli M. Research review: The role of obstetric and neonatal complications in childhood attention deficit and hyperactivity disorder - A systematic review. J Child Psychol Psychiatr. 2017;58:1290–1300. doi: 10.1111/jcpp.12779. DOI: https://doi.org/10.1111/jcpp.12779
Momany AM, Kamradt JM, Nikolas MA. A meta-analysis of the association between birth weight and attention deficit hyperactivity disorder. J Abnorm Child Psychol. 2018;46:1409–1426. doi: 10.1007/S10802-017-0371-9. DOI: https://doi.org/10.1007/s10802-017-0371-9
Manzari N, Matvienko-Sikar K, Baldoni F, O’Keeffe GW, Khashan AS. Prenatal maternal stress and risk of neurodevelopmental disorders in the offspring: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2019;54:1299–1309. doi: 10.1007/S00127-019-01745-3. DOI: https://doi.org/10.1007/s00127-019-01745-3
Franke B, Faraone SV, Asherson P, Buitelaar J, Bau CHD, Ramos-Quiroga JA, et al. The genetics of attention deficit/hyperactivity disorder in adults, a review. Mol Psychiatr. 2011;17:960–987. doi: 10.1038/mp.2011.138. DOI: https://doi.org/10.1038/mp.2011.138
Starck M, Grünwald J, Schlarb AA. Occurrence of ADHD in parents of ADHD children in a clinical sample. Neuropsychiatr Dis Treat. 2016;12:581-588. doi: 10.2147/ndt.s100238. DOI: https://doi.org/10.2147/NDT.S100238
Lindström K, Lindblad F, Hjern A. Preterm birth and attention-deficit/hyperactivity disorder in schoolchildren. Pediatrics. 2011;127:858–865. doi: org/10.1542/peds.2010-1279. DOI: https://doi.org/10.1542/peds.2010-1279
Neuman RJ, Lobos E, Reich W, Henderson CA, Sun LW, Todd RD. Prenatal smoking exposure and dopaminergic genotypes interact to cause a severe ADHD subtype. Biol Psychiatr. 2007;61:1320–1328. doi: 10.1016/j.biopsych.2006.08.049. DOI: https://doi.org/10.1016/j.biopsych.2006.08.049
Huang L, Wang Y, Zhang L, Zheng Z, Zhu T, Qu Y, et al. Maternal smoking and attention-deficit/hyperactivity disorder in offspring: A meta-analysis. Pediatrics. 2018;141. doi: 10.1542/peds.2017-2465/77142. DOI: https://doi.org/10.1542/peds.2017-2465
Cornelius ME, Loretan CG, Jamal A, Davis Lynn BC, Mayer M, Alcantara IC, et al. Tobacco product use among adults – United States, 2021. Morb Mortal Wkly Rep. 2023;72:475–483. doi: 10.15585/mmwr.mm7218A1. DOI: https://doi.org/10.15585/mmwr.mm7218a1
Pagnin D, Zamboni Grecco ML, Furtado EF. Prenatal alcohol use as a risk for attention-deficit/hyperactivity disorder. Eur Arch Psychiatry Clin Neurosci. 2019;269:681–687. doi: 10.1007/S00406-018-0946-7/metrics. DOI: https://doi.org/10.1007/s00406-018-0946-7
Fliers EA, Buitelaar JK, Maras A, Bul K, Höhle E, Faraone SV, et al. ADHD is a risk factor for overweight and obesity in children. J Devel Behav Pediatr. 2013;34:566–574. doi: 10.1097/DBP.0b013e3182a50a67. DOI: https://doi.org/10.1097/DBP.0b013e3182a50a67
Sciberras E, Mulraney M, Silva D, Coghill D. Prenatal risk factors and the etiology of ADHD-Review of existing evidence. Curr Psychiatry Rep. 2017;19:1–1. doi: 10.1007/S11920-017-0753-2. DOI: https://doi.org/10.1007/s11920-017-0753-2
Hawi Z, Cummins TDR, Tong J, Arcos-Burgos M, Zhao Q, Matthews N, et al. Rare DNA variants in the brain-derived neurotrophic factor gene increase risk for attention-deficit hyperactivity disorder: a next-generation sequencing study. Mol Psychiatr. 2017;22:580–584. doi: 10.1038/MP.2016.117. DOI: https://doi.org/10.1038/mp.2016.117
Rydell M, Taylor MJ, Larsson H. Genetic and environmental contributions to the association between ADHD and affective problems in early childhood-A Swedish population-based twin study. Am J Med Genet B Neuropsychiatr Genet. 2017;174:538–546. doi: 10.1002/ajmg.b.32536. DOI: https://doi.org/10.1002/ajmg.b.32536
Capusan AJ, Bendtsen P, Marteinsdottir I, Kuja-Halkola R, Larsson H. Genetic and environmental contributions to the association between attention deficit hyperactivity disorder and alcohol dependence in adulthood: A large population-based twin study. Am J Med Genet B Neuropsychiatr Genet. 2015;168:414–422. doi: 10.1002/ajmg.b.32300. DOI: https://doi.org/10.1002/ajmg.b.32300
Greven CU, Rijsdijk FV, Plomin R. A twin study of ADHD symptoms in early adolescence: hyperactivity-impulsivity and inattentiveness show substantial genetic overlap but also genetic specificity. J Abnorm Child Psychol. 2011;39:265–275. doi: 10.1007/S10802-010-9451-9. DOI: https://doi.org/10.1007/s10802-010-9451-9
Luo Y, Weibman D, Halperin JM, Li X. A Review of heterogeneity in attention deficit/hyperactivity disorder (ADHD). Front Hum Neurosci. 2019;13. doi: 10.3389/fnhum.2019.00042. DOI: https://doi.org/10.3389/fnhum.2019.00042
Karalunas SL, Nigg JT. Heterogeneity and subtyping in attention-deficit/hyperactivity disorder—Considerations for emerging research using person-centered computational approaches. Biol Psychiatr. 2020;88:103–110. doi: 10.1016/j.biopsych.2019.11.002. DOI: https://doi.org/10.1016/j.biopsych.2019.11.002
Vaidya CJ, You X, Mostofsky S, Pereira F, Berl MM, Kenworthy L. Data-driven identification of subtypes of executive function across typical development, attention deficit hyperactivity disorder, and autism spectrum disorders. J Child Psychol Psychiatr. 2020;61:51–61. doi: 10.1111/jcpp.13114. DOI: https://doi.org/10.1111/jcpp.13114
Wolfers T, Beckmann CF, Hoogman M, Buitelaar JK, Franke B, Marquand AF. Individual differences v. the average patient: mapping the heterogeneity in ADHD using normative models. Psychol Med. 2020;50:314–323. doi: 10.1017/S0033291719000084. DOI: https://doi.org/10.1017/S0033291719000084
Wray NR, Wijmenga C, Sullivan PF, Yang J, Visscher PM. Common disease is more complex than implied by the core gene omnigenic model. Cell. 2018;173:1573–1580. doi: 10.1016/j.cell.2018.05.051. DOI: https://doi.org/10.1016/j.cell.2018.05.051
Nigg JT, Karalunas SL, Feczko E, Fair DA. Toward a revised nosology for attention-deficit/hyperactivity disorder heterogeneity. Biol Psychiatry Cogn Neurosci Neuroimaging. 2020;5:726–737. doi: 10.1016/j.bpsc.2020.02.005. DOI: https://doi.org/10.1016/j.bpsc.2020.02.005
Xu G, Strathearn L, Liu B, Yang B, Bao W. Twenty-year trends in diagnosed attention-deficit/hyperactivity disorder among US children and adolescents, 1997-2016. JAMA Netw Open. 2018;1. doi: 10.1001/jamanetworkopen.2018.1471. DOI: https://doi.org/10.1001/jamanetworkopen.2018.1471
Auvin S, Wirrell E, Donald KA, Berl M, Hartmann H, Valente KD, et al. Systematic review of the screening, diagnosis, and management of ADHD in children with epilepsy. Consensus paper of the Task Force on Comorbidities of the ILAE Pediatric Commission. Epilepsia. 2018;59:1867–1880. doi: 10.1111/epi.14549. DOI: https://doi.org/10.1111/epi.14549
Foy JM, Earls MF. A process for developing community consensus regarding the diagnosis and management of attention-deficit/hyperactivity disorder. Pediatrics. 2005;115. doi: 10.1542/peds.2004-0953. DOI: https://doi.org/10.1542/peds.2004-0953
Mulraney M, Arrondo G, Musullulu H, Iturmendi-Sabater I, Cortese S, Westwood SJ, et al. Systematic review and meta-analysis: Screening tools for attention-deficit/hyperactivity disorder in children and adolescents. J Am Acad Child Adolesc Psychiatr. 2022;61:982–996. doi: 10.1016/j.jaac.2021.11.031. DOI: https://doi.org/10.1016/j.jaac.2021.11.031
Steingard R, Taskiran S, Connor DF, Markowitz JS, Stein MA. New formulations of stimulants: An update for clinicians. J Child Adolesc Psychopharmacol. 2019;29:324. doi: 10.1089/cap.2019.0043. DOI: https://doi.org/10.1089/cap.2019.0043
Budur K, Mathews M, Adetunji B, Mathews M, Mahmud J. Non-stimulant treatment for attention deficit hyperactivity disorder. Psychiatry (Edgmont). 2005;2:44.
Cândido RCF, Menezes de Padua CA, Golder S, Junqueira DR. Immediate‐release methylphenidate for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database Syst Rev. 2021;2021. doi: 10.1002/14651858.CD013011.PUB2. DOI: https://doi.org/10.1002/14651858.CD013011.pub2
Jaeschke RR, Sujkowska E, Sowa-Kućma M. Methylphenidate for attention-deficit/hyperactivity disorder in adults: a narrative review. Psychopharmacology. 2021;238:2667–2691. doi: 10.1007/S00213-021-05946-0. DOI: https://doi.org/10.1007/s00213-021-05946-0
Faraone SV, Spencer T, Aleardi M, Pagano C, Biederman J. Meta-analysis of the efficacy of methylphenidate for treating adult attention-deficit/hyperactivity disorder. J Clin Psychopharmacol. 2004;24. doi: 10.1097/01.jcp.0000108984.11879.95. DOI: https://doi.org/10.1097/01.jcp.0000108984.11879.95
Faraone SV, Buitelaar J. Comparing the efficacy of stimulants for ADHD in children and adolescents using meta-analysis. Eur Child Adolesc Psychiatr. 2010;19:353–364. doi: 10.1007/S00787-009-0054-3. DOI: https://doi.org/10.1007/s00787-009-0054-3
Markowitz JS, Straughn AB, Patrick KS. Advances in the pharmacotherapy of attention-deficit-hyperactivity disorder: focus on methylphenidate formulations. Pharmacotherapy. 2003;23:1281–1299. doi: 10.1592/phco.23.12.1281.32697. DOI: https://doi.org/10.1592/phco.23.12.1281.32697
Mattingly GW, Wilson J, Ugarte L, Glaser P. Individualization of attention-deficit/hyperactivity disorder treatment: pharmacotherapy considerations by age and co-occurring conditions. CNS Spectr. 2021;26(3):202-221. doi: 10.1017/S1092852919001822. DOI: https://doi.org/10.1017/S1092852919001822
Maneeton N, Maneeton B, Woottiluk P, Suttajit S, Likhitsathian S, Charnsil C, et al. Comparative efficacy, acceptability, and tolerability of dexmethylphenidate versus placebo in child and adolescent ADHD: A meta-analysis of randomized controlled trials. Neuropsychiatr Dis Treat. 2015;11:2943–2952. doi: 10.2147/ndt.S91765. DOI: https://doi.org/10.2147/NDT.S91765
Stein MA, Waldman ID, Charney E, Aryal S, Sable C, Gruber R, et al. Dose effects and comparative effectiveness of extended release dexmethylphenidate and mixed amphetamine salts. J Child Adolesc Psychopharmacol. 2011;21(6):581-588. doi: 10.1089/cap.2011.0018. DOI: https://doi.org/10.1089/cap.2011.0018
Ermer JC, Pennick M, Frick G. Lisdexamfetamine dimesylate: Prodrug delivery, Amphetamine exposure and duration of efficacy. Clin Drug Investig. 2016;36:341–356. doi: 10.1007/S40261-015-0354-Y/FIGURES/4. DOI: https://doi.org/10.1007/s40261-015-0354-y
Elbe D, Macbride A, Reddy D. Focus on lisdexamfetamine: A review of its use in child and adolescent psychiatry. J Can Acad Child Adolesc Psychiatry. 2010;19(4):303-314. PMID: 21037922.
Wigal SB, Kollins SH, Childress AC, Squires L, Brams M, Childress A, et al. A 13-hour laboratory school study of lisdexamfetamine dimesylate in school-aged children with attention-deficit/hyperactivity disorder. Child Adolesc Psychiatry Ment Health. 2009;3:17. doi; 10.1186/1753-2000-3-17. DOI: https://doi.org/10.1186/1753-2000-3-17
Levine J, Swanson H. The use of lisdexamfetamine to treat ADHD in a patient with stimulant (methamphetamine) use disorder. Case Rep Psychiatry. 2023;2023. doi: 10.1155/2023/5574677. DOI: https://doi.org/10.1155/2023/5574677
Radonjić NV, Bellato A, Khoury NM, Cortese S, Faraone S V. Nonstimulant medications for attention-deficit/hyperactivity disorder (ADHD) in adults: Systematic review and meta-analysis. CNS Drugs. 2023;37:381–397. doi: 10.1007/S40263-023-01005-8. DOI: https://doi.org/10.1007/s40263-023-01005-8
Sveinsdóttir HS, Christensen C, Þorsteinsson H, Lavalou P, Parker MO, Shkumatava A, et al. Novel non-stimulants rescue hyperactive phenotype in an adgrl3.1 mutant zebrafish model of ADHD. Neuropsychopharmacology. 2022;48:1155-1163. doi: 10.1038/s41386-022-01505-z. DOI: https://doi.org/10.1038/s41386-022-01505-z
Idrees I, Bellato A, Cortese S, Groom MJ. The effects of stimulant and non-stimulant medications on the autonomic nervous system (ANS) functioning in people with ADHD: A systematic review and meta-analysis. Neurosci Biobehav Rev. 2023;144:104968. doi: 10.1016/j.neubiorev.2022.104968. DOI: https://doi.org/10.1016/j.neubiorev.2022.104968
McCabe SE, Schulenberg JE, Wilens TE, Schepis TS, McCabe VV, Veliz PT. Cocaine or methamphetamine use during young adulthood following stimulant use for attention-deficit/hyperactivity disorder during adolescence. JAMA Netw Open. 2023;6:e2322650. doi: 10.1001/jamanetworkopen.2023.22650. DOI: https://doi.org/10.1001/jamanetworkopen.2023.22650
Schepis TS, Werner KS, Figueroa O, McCabe VV, Schulenberg JE, Veliz PT, et al. Type of medication therapy for ADHD and stimulant misuse during adolescence: a cross-sectional multi-cohort national study. EClinicalMedicine. 2023;58. doi: 10.1016/j.eclinm.2023.101902. DOI: https://doi.org/10.1016/j.eclinm.2023.101902
McCabe SE, Figueroa O, McCabe VV, Schepis TS, Schulenberg JE, Veliz PT, et al. Is age of onset and duration of stimulant therapy for ADHD associated with cocaine, methamphetamine, and prescription stimulant misuse? J Child Psychol Psychiatry. 2024;65:100–111. doi: 10.1111/jcpp.13807. DOI: https://doi.org/10.1111/jcpp.13807
Wolraich ML, Chan E, Froehlich T, Lynch RL, Bax A, Redwine ST, et al. ADHD diagnosis and treatment guidelines: A historical perspective. Pediatrics. 2019;144. doi: 10.1542/peds.2019-1682. DOI: https://doi.org/10.1542/peds.2019-1682
Fullen T, Jones SL, Emerson LM, Adamou M. Psychological treatments in adult ADHD: A systematic review. J Psychopathol Behav Assess. 2020;42:500–518. doi: 10.1007/s10862-020-09794-8. DOI: https://doi.org/10.1007/s10862-020-09794-8
Cabral MDI, Liu S, Soares N. Attention-deficit/hyperactivity disorder: diagnostic criteria, epidemiology, risk factors and evaluation in youth. Transl Pediatr. 2020;9:S104–113. doi: 10.21037/tp.2019.09.08. DOI: https://doi.org/10.21037/tp.2019.09.08
Haddad HW, Hankey PB, Ko J, Eswani Z, Bhatti P, Edinoff AN, et al. Viloxazine, a non-stimulant norepinephrine reuptake inhibitor, for the treatment of attention deficit hyperactivity disorder: A 3 year update. Health Psychol Res. 2022;10. doi; 10.52965/001C.37018. DOI: https://doi.org/10.52965/001c.37018
Havdahl A, Wootton RE, Leppert B, Riglin L, Ask H, Tesli M, et al. Associations between pregnancy-related predisposing factors for offspring neurodevelopmental conditions and parental genetic liability to attention-deficit/hyperactivity disorder, Autism, and schizophrenia: The Norwegian mother, father and child cohort study (MoBa). JAMA Psychiatry. 2022;79. doi: 10.1001/jamapsychiatry.2022.1728. DOI: https://doi.org/10.1001/jamapsychiatry.2022.1728
Neugebauer J, Wittsiepe J, Kasper-Sonnenberg M, Schöneck N, Schölmerich A, Wilhelm M. The influence of low level pre- and perinatal exposure to PCDD/Fs, PCBs, and lead on attention performance and attention-related behavior among German school-aged children: results from the Duisburg Birth Cohort Study. Int J Hyg Environ Health. 2015;218:153–162. doi: 10.1016/j.ijheh.2014.09.005. DOI: https://doi.org/10.1016/j.ijheh.2014.09.005
Abid Z, Roy A, Herbstman JB, Ettinger AS. Urinary polycyclic aromatic hydrocarbon metabolites and attention/deficit hyperactivity disorder, learning disability, and special education in U.S. children aged 6 to 15. J Environ Public Health. 2014;2014. doi: 10.1155/2014/628508. DOI: https://doi.org/10.1155/2014/628508
Perera FP, Wheelock K, Wang Y, Tang D, Margolis AE, Badia G, et al. Combined effects of prenatal exposure to polycyclic aromatic hydrocarbons and material hardship on child ADHD behavior problems. Environ Res. 2018;160:506–5013. doi: 10.1016/j.envres.2017.09.002. DOI: https://doi.org/10.1016/j.envres.2017.09.002
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











