Smoking Trends, Influencers, and Attitudes Among Future Medical Professionals
DOI:
https://doi.org/10.54133/ajms.v9i2.2320Keywords:
Attitudes, Influencing factors, Medical students, Smoking, University of BaghdadAbstract
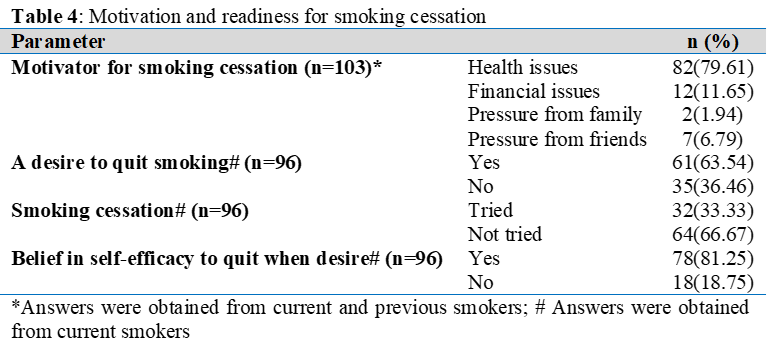
Background: While medical students should model healthy behaviors, smoking is common among them. Data on smoking among Iraqi medical students remains limited. Objective: To determine the prevalence, attitudes, and influencing factors for smoking among Iraqi medical students. Methods: A cross-sectional study was conducted from December 2024 to March 2025, involving 250 medical students at Baghdad University. Participants completed a self-administered questionnaire that was newly developed based on relevant literature and validated by a panel of experts. The developed questionnaire was designed to assess smoking status and its influencing factors, attitudes towards smoking, quitting behavior and its influencing factors. Results: Participants' mean age was 21.02±2.16 years; most were single (93.2%) females (58.4%). 41.2% of participants smoked at least once in their life, with 52.42% of those being daily smokers. Cigarettes and hookah were the most tried smoking methods. Peer influence (29%) and stress (24%) were cited as smoking motivators. Additionally, male gender, older age, enrollment in Medicine College, higher academic level, and greater family income were all significantly linked to smoking trials. While 79.61% of smoking participants cited health issues as a quitting motivator, only 33.33% had tried to quit. Most participants had negative attitudes towards smoking. Conclusions: Smoking is highly prevalent among Iraqi medical students despite their negative attitudes towards it. Male gender, older age, enrollment in medical college, higher academic levels, greater family income, peer pressure, and stress increase smoking likelihood. Health concerns serve as motivators for smoking cessation; however, few smokers have attempted to quit.
Downloads
References
Kim J, Song H, Lee J, Kim YJ, Chung HS, Yu JM, etal. Smoking and passive smoking increases mortality through mediation effect of cadmium exposure in the United States. Sci Rep. 2023;13(1):3878. doi: 10.1038/s41598-023-30988-z. DOI: https://doi.org/10.1038/s41598-023-30988-z
Global Adult Tobacco Survey Collaborative Group. Global Adult Tobacco Survey (GATS): Core questionnaire with optional questions, version 2.0. Atlanta, GA: Centers for Disease Control and Prevention; 2016-2020.
Abubaker A, Alrefaie A, Jum'a M, Al-Azaideh B, Alitelat A, Alajmi H, et al. Status of smoking research in Jordan: Scoping review and evidence synthesis. High Yield Med Rev.2023;1(1). doi:10.59707/hymrILSQ2807. DOI: https://doi.org/10.59707/hymrILSQ2807
Maziak W, Nakkash R, Bahelah R, Husseini A, Fanous N, Eissenberg T. Tobacco in the Arab world: old and new epidemics amidst policy paralysis. Health Policy Plan. 2014;29(6):784-794. doi:10.1093/heapol/czt055. DOI: https://doi.org/10.1093/heapol/czt055
Noori CM, Hama Saeed MA, Chitheer T, Ali AM, Ali KM, Jader JA, et al. Prevalence of smoking habits among the Iraqi population in 2021. Public Health Toxicol.2024;4(4):20. doi:10.18332/pht/197277. DOI: https://doi.org/10.18332/pht/197277
Alotaibi SA, Durgampudi PK. Factors associated with tobacco smoking among Saudi college students: A systematic review. Tobacco Prevent Cessation.2020;6:36. doi: 10.18332/tpc/122444. DOI: https://doi.org/10.18332/tpc/122444
Jawad M, Lee JT, Millett C. Waterpipe tobacco smoking prevalence and correlates in 25 Eastern Mediterranean and Eastern European Countries: Cross-sectional analysis of the global youth tobacco survey. Nicotine Tob Res. 2016;18(4):395-402. doi: 10.1093/ntr/ntv101. DOI: https://doi.org/10.1093/ntr/ntv101
World Health Organization. WHO report on the global tobacco epidemic, 2019: country profile United Arab Emirates. Geneva: World Health Organization; 2019.
Sarkees AN, Issa SA. Smoking behaviors and related factors among secondary school students in Duhok city. Iraqi J Pharmacy. 2024;21(1):36-44. doi: 10.33899/iraqij.p.2024.145584.1077. DOI: https://doi.org/10.33899/iraqij.p.2024.145584.01077
Warren CW, Sinha DN, Lee J, Lea V, Jones NR. Tobacco use, exposure to secondhand smoke, and cessation counseling among medical students: cross-country data from the Global Health Professions Student Survey (GHPSS), 2005-2008. BMC Public Health. 2011;11:1-6. doi:10.1186/1471-2458-11-72. DOI: https://doi.org/10.1186/1471-2458-11-72
Khan FM, Husain SJ, Laeeq A, Awais A, Hussain SF, Khan JA. Smoking prevalence, knowledge and attitudes among medical students in Karachi, Pakistan. East Mediterr Health J. 2005;11(5-6):952-958. PMID: 16761665.
Gupta H, Gupta S, Rozatkar A. Magnitude of substance use and its associated factors among the medical students in India and implications for medical education: A narrative review. Indian J Psychol Med. 2021;44:1–9. doi:10.1177/02537176211032366. DOI: https://doi.org/10.1177/02537176211032366
Alkhalaf M, Suwyadi A, AlShamakhi E, Oribi H, Theyab Z, Sumayli I, et al. Determinants and prevalence of tobacco smoking among medical students at Jazan University, Saudi Arabia. J Smok Cessation. 2021;2021:e20. doi:10.1155/2021/6632379. DOI: https://doi.org/10.1155/2021/6632379
Othman SM, Saleh AM, Ali KB. Prevalence of cigarette smoking among Hawler medical university students. Zanco J Med Sci. 2009;13(2):57-62. doi: 10.15218/zjms.2009.020. DOI: https://doi.org/10.15218/zjms.2009.020
Yasso FS, Yaso SS, Yasso PS, Dafdony IV. Prevalence of cigarette smoking among medical Iraqi students. Am J Public Health Res. 2014;2(215):2691. doi:10.12691/ajphr-2-1-3. DOI: https://doi.org/10.12691/ajphr-2-1-3
Pazdro-Zastawny K, Dorobis K, Bobak-Sarnowska E, Zatoński T. Prevalence and associated factors of cigarette smoking among medical students in Wroclaw, Poland. Risk Manag Healthc Policy. 2022;15:509-519. doi:10.2147/RMHP.S346619. DOI: https://doi.org/10.2147/RMHP.S337529
Imamuzzaman M, Muhammad F, Haque MI, Ahmed K, Mukta KF, Reuben RF, et al. Prevalence of smoking and its associated factors among adolescent males in Bangladesh: A community survey. Open Public Health J. 2022;15:e187494452211040.doi:10.2174/18749445-v15-e221115-2022-83. DOI: https://doi.org/10.2174/18749445-v15-e221115-2022-83
Abdelraouf MMF, Abdalla RAM, Mohamed DMS, Ahmed AKA, Abuzaid MAM, Issak MA, et al. Prevalence of smoking and its associated factors among students at the University of Dongola, Northern State, Sudan: A cross-sectional study. Ann Med Surg (Lond). 2024;86(5):2543-2548. doi: 10.1097/MS9.0000000000001862. DOI: https://doi.org/10.1097/MS9.0000000000001862
Todorović I, Cheng F, Stojisavljević S, Marinković S, Kremenović S, Savić P, et al. Prevalence of cigarette smoking and influence of associated factors among students of the university of Banja Luka: A cross-sectional study. Medicina (Kaunas). 2022;58(4):502. doi: 10.3390/medicina58040502. DOI: https://doi.org/10.3390/medicina58040502
Zubair OA. Prevalence of smoking among school students in Iraq. Cureus. 2024;16(8):e67048. doi:10.7759/cureus.67048. DOI: https://doi.org/10.7759/cureus.67048
World Health Organization. Global Youth Tobacco Survey [Internet]. 2023 [cited 2025 Mar]. Available from: http://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/global-youth-tobacco-survey
Memon MA, Ting H, Cheah JH, Thurasamy R, Chuah F, Cham TH. Sample size for survey research: review and recommendations. J Appl Struct Equ Modeling. 2020;4(2):1-20. doi: 10.47263/JASEM.4(2)01. DOI: https://doi.org/10.47263/JASEM.4(2)01
Al-Kaabba AF, Saeed AA, Abdalla AM, Hassan HA, Mustafa AA. Prevalence and associated factors of cigarette smoking among medical students at King Fahad Medical City in Riyadh of Saudi Arabia. J Fam Commun Med. 2011;18(1):8-12. doi: 10.4103/1319-1683.78631. DOI: https://doi.org/10.4103/1319-1683.78631
Jarelnape AA, Ahmed W, Omer S, Fadlala A, Ali Z, Hassan M, et al. Prevalence of smoking cigarettes and beliefs regarding smoking habits among medical students: a cross-sectional study in Sudan. Front Public Health. 2023;11:1193475. doi: 10.3389/fpubh.2023.1193475 25. DOI: https://doi.org/10.3389/fpubh.2023.1193475
Aslan D, Ay P, Raymond K, Aşut Ö, Abuduxike G, Şengelen M, et al. Medicalstudents’ tobacco consumption status and experiences with smoke-free law violations in enclosed spaces in Türkiye and Northern Cyprus. Thorac Res Pract. 2025;26(2):48. doi: 10.4274/ThoracResPract.2024.24084. DOI: https://doi.org/10.4274/ThoracResPract.2024.24084
Hassan MKR. Factors affecting urbanisation in Iraq: A historical analysis from 1921 to the present. Urbanisation.2023;8(1):61–78. doi:10.1177/24557471231169386. DOI: https://doi.org/10.1177/24557471231169386
Aljunaid MA, Mehdar SA, Bukhari HS, AlSharif RH, AlSharif RH, AlHarbi S. Exploring cognitive and behavioral changes related to smoking among medical students in Saudi Arabia: A cross-sectional study. Medicina (Kaunas). 2024;60(12):1935. doi: 10.3390/medicina60121935. DOI: https://doi.org/10.3390/medicina60121935
Fares J, Saadeddin Z, Al Tabosh H, Aridi H, El Mouhayyar C, Koleilat MK, et al. Extracurricular activities associated with stress and burnout in preclinical medical students. J Epidemiol Glob Health. 2016;6(3):177–185. doi: 10.1016/j.jegh.2015.10.003. DOI: https://doi.org/10.1016/j.jegh.2015.10.003
Khader YS, Alsadi AA. Smoking habits among university students in Jordan: prevalence and associated factors. East Mediterr Health J. 2008;14(4):897-904. PMID: 19166173.
Boopathirajan R, Muthunarayanan L. Awareness, attitude and use of tobacco among medical students in Chennai. J Lifestyle Med. 2017;7(1):27-34. doi: 10.15280/jlm.2017.7.1.27. DOI: https://doi.org/10.15280/jlm.2017.7.1.27
Jirdi MA. Prevalence of smoking habit and associated factors among of Al-Andalus University of medical science. Tishreen univ J Res Sci Stud Health Sci Ser. 2018;40(5):103.
Alnasser AHA, Al-Tawfiq JA, Kheimi RMA, Alibrahim RMS, Albanawi NAH, Almeshal AKA, et al. Gender differences in smoking attitude among Saudi Medical students. Asian Pac J Cancer Prev. 2022;23(6):2089-2093. doi: 10.31557/APJCP.2022.23.6.2089. DOI: https://doi.org/10.31557/APJCP.2022.23.6.2089
Al-Kubaisy W, Abdullah NN, Al-Nuaimy H, Halawany G, Kurdy S. Epidemiological study on tobacco smoking among university students in Damascus, Syrian Arab Republic. East Mediterr Health J. 2012;18(7):723-727. doi: 10.26719/2012.18.7.23. DOI: https://doi.org/10.26719/2012.18.7.23
Von Ah D, Ebert S, Ngamvitroj A, Park N, Kang DH. Factors related to cigarette smoking initiation and use among college students. Tob Induc Dis. 2005;3(1):27-40. doi: 10.1186/1617-9625-3-1-27. DOI: https://doi.org/10.1186/1617-9625-3-1-27
Seemadevi T, Naganandini S, Luke AM, Hamad Ingafou MS. Smoking trends and awareness among Indian University students: A qualitative study. Heliyon. 2025;11;e41078. doi:10.1016/j.heliyon.2024.e41078. DOI: https://doi.org/10.1016/j.heliyon.2024.e41078
Dadipoor S, Kok G, Aghamolaei T, Heyrani A, Ghaffari M, Ghanbarnezhad A. Factors associated with hookah smoking among women: A systematic review. Tob Prev Cessation. 2019;5:26. doi:10.18332/tpc/110586. DOI: https://doi.org/10.18332/tpc/110586
Ahmed SM. Prevalence and perceptions toward electronic cigarettes (vaping) use among medical students: A new public health challenge in Kurdistan Region, Iraq. J Med Chem Sci. 2024;7(5): 720-728.
Eden VR, Hamid H, Das S, Dioso R. Trend and awareness of e-cigarettes among students in a private college in Sabah Malaysia. AUIQ ComplBiol Syst. 2024;1(2):86-95. doi: 10.70176/3007-973X.1018. DOI: https://doi.org/10.70176/3007-973X.1018
Ahmed LA, Verlinden M, Alobeidli MA, Alahbabi RH, AlKatheeri R, Saddik B, et al. Patterns of tobacco smoking and nicotine vaping among university students in the United Arab Emirates: a cross-sectional study. Int J Environ Res Public Health. 2021;18(14):7652. doi: 10.3390/ijerph18147652. DOI: https://doi.org/10.3390/ijerph18147652
Castaldelli-Maia JM, Ventriglio A, Bhugra D. Tobacco smoking: From 'glamour' to 'stigma'. A comprehensive review. Psychiatry Clin Neurosci. 2016;70(1):24-33. doi: 10.1111/pcn.12365. DOI: https://doi.org/10.1111/pcn.12365
Al-Dhafri S. Smoking among Sultan Qaboos University students: Prevalence rates, attitudes, causes and treatment. J Arts Soc Sci. 2019;10(1):5. DOI: https://doi.org/10.53542/jass.v10i1.3212
Qasem NW, Al-Omoush BH, Altbeinat SK, Al-Dlaijem MM, Salahat RI, Okour SA. Smoking cessation rate and predictors of successful quitting in Jordan: A cross-sectional study. Medicine. 2024 ;103(27):e38708. doi:10.1097/MD.0000000000038708. DOI: https://doi.org/10.1097/MD.0000000000038708
Al-Jayyousi GF, Shraim M, Hassan DA, Al-Hamdani M, Kurdi R, Hamad NA, et al. University students’ and staff attitudes toward the implementation of a tobacco-free policy: a view from Qatar. Prev Med Rep. 2024;38:102605. doi: 10.1016/j.pmedr.2024.102605. DOI: https://doi.org/10.1016/j.pmedr.2024.102605
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











