High Levels of Depression Among Healthcare Workers Four Years After the COVID-19 Pandemic: A Cross-Sectional Survey from a High-Workload, Deteriorating Healthcare System
DOI:
https://doi.org/10.54133/ajms.v9i2.2317Keywords:
COVID-19, Depression, Healthcare workers, Iraq, Mental health, Occupational stress, PHQ-9.Abstract
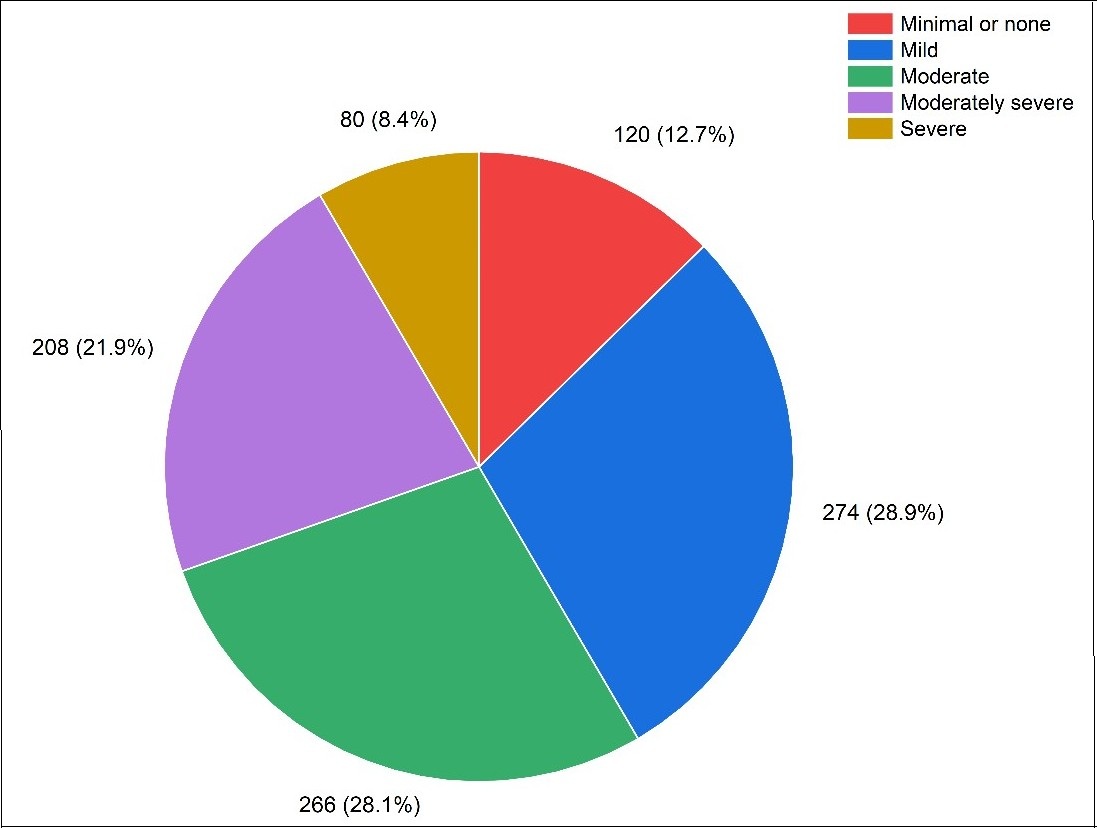
Background: Healthcare workers (HCWs) in Iraq have endured significant psychological burdens throughout the COVID-19 pandemic. Despite the prolonged impact of the pandemic, studies evaluating the long-term mental health consequences among HCWs remain scarce. To our knowledge. Objective: To assess the psychological impact of the COVID-19 pandemic on HCWs four years after the pandemic. Methods: A cross-sectional study was conducted between May and December 2024. The Patient Health Questionnaire-9 (PHQ-9) was utilized to evaluate depression. Multiple logistic regressions were performed to identify factors independently associated with depression. Results: 948 HCWs were included in this study. 60.3% of them were female, with a mean age of 28.81 years. We found a high level of depression, with 69.4% of HCWs being affected. Younger and single HCWs had a higher depression rate, with a prevalence of 67.4% and 74.3%, respectively. Higher levels of depression were associated with lower educational attainment (84.1%). Also, those with a history of medical, psychological, or family psychological conditions were strongly associated with higher depression levels. Depression affected 72.9% of individuals who had experienced COVID-19 infection before. Medical staff working on the frontlines showed particularly high depression rates at 80.3%. The mild and moderate depression symptoms were most common, since they affected 28.9% and 28.1%, respectively. Conclusions: For the first time in Iraq, this study revealed that 69.4% of healthcare workers (HCWs) suffered from depression four years after the COVID-19 pandemic. Depression was more prevalent among doctors or nurses and those with lower educational attainment.
Downloads
References
Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020 Feb 15;395(10223):470-473. doi: 10.1016/S0140-6736(20)30185-9. DOI: https://doi.org/10.1016/S0140-6736(20)30185-9
Mahase E. China coronavirus: WHO declares international emergency as death toll exceeds 200. BMJ. 2020;368:m408. doi: 10.1136/bmj.m408. DOI: https://doi.org/10.1136/bmj.m408
JHU J. Johns Hopkins university coronavirus resource center.[Online] Available at: https://coronavirus.jhu.edu/map.html. Accessed; 2025.
Mawlood NA, Lafta RK. Trends in COVID-19: Incidence, mortality, and case fatality in Iraq. Saudi Med J. 2022;43(5):500-507. doi: 10.15537/smj.2022.43.5.20220088. DOI: https://doi.org/10.15537/smj.2022.43.5.20220088
World Health Organization. Weekly epidemiological update on COVID-19-3. August 2023. Available at: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---3-august-2023
Steffens NK, LaRue CJ, Haslam C, Walter ZC, Cruwys T, Munt KA, et al. Social identification-building interventions to improve health: a systematic review and meta-analysis. Health Psychol Rev. 2021;15(1):85-112. doi: 10.1080/17437199.2019.1669481. DOI: https://doi.org/10.1080/17437199.2019.1669481
Razu SR, Yasmin T, Arif TB, Islam MS, Islam SMS, Gesesew HA, et al. Challenges faced by healthcare professionals during the COVID-19 pandemic: A qualitative inquiry from bangladesh. Front Public Health. 2021;9:647315. doi: 10.3389/fpubh.2021.647315. DOI: https://doi.org/10.3389/fpubh.2021.647315
De Kock JH, Latham HA, Leslie SJ, Grindle M, Munoz SA, Ellis L, et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health. 2021;21(1):104. doi: 10.1186/s12889-020-10070-3. DOI: https://doi.org/10.1186/s12889-020-10070-3
Taylor S, Landry CA, Rachor GS, Paluszek MM, Asmundson GJG. Fear and avoidance of healthcare workers: An important, under-recognized form of stigmatization during the COVID-19 pandemic. J Anxiety Disord. 2020;75:102289. doi: 10.1016/j.janxdis.2020.102289. DOI: https://doi.org/10.1016/j.janxdis.2020.102289
Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976. DOI: https://doi.org/10.1001/jamanetworkopen.2020.3976
Juliana N, Mohd Azmi NAS, Effendy N, Mohd Fahmi Teng NI, Azmani S, et al. Exploring the Associated factors of depression, anxiety, and stress among healthcare shift workers during the COVID-19 pandemic. Int J Environ Res Public Health. 2022;19(15):9420. doi: 10.3390/ijerph19159420. DOI: https://doi.org/10.3390/ijerph19159420
Tong F, Zhang L, Huang L, Yang H, Wen M, Jiang L, et al. The psychological impact of COVID-19 pandemic on healthcare workers. Front Public Health. 2022;10:963673. doi: 10.3389/fpubh.2022.963673. DOI: https://doi.org/10.3389/fpubh.2022.963673
Wu T, Jia X, Shi H, Niu J, Yin X, Xie J, et al. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J Affect Disord. 2021;281:91-98. doi: 10.1016/j.jad.2020.11.117. DOI: https://doi.org/10.1016/j.jad.2020.11.117
Chan AO, Huak CY. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup Med (Lond). 2004;54(3):190-196. doi: 10.1093/occmed/kqh027. DOI: https://doi.org/10.1093/occmed/kqh027
Kang P, Lv Y, Hao L, Tang B, Liu Z, Liu X, et al. Psychological consequences and quality of life among medical rescuers who responded to the 2010 Yushu earthquake: A neglected problem. Psychiatry Res. 2015;230(2):517-23. doi: 10.1016/j.psychres.2015.09.047. DOI: https://doi.org/10.1016/j.psychres.2015.09.047
Tiong WW, Koh GC. Ethical considerations in the review of Singapore's H1N1 pandemic response framework in 2009. Ann Acad Med Singap. 2013;42(5):246-50. PMID: 23771113. DOI: https://doi.org/10.47102/annals-acadmedsg.V42N5p246
Kunz M, Strasser M, Hasan A. Impact of the coronavirus disease 2019 pandemic on healthcare workers: systematic comparison between nurses and medical doctors. Curr Opin Psychiatry. 2021;34(4):413-419. doi: 10.1097/YCO.0000000000000721. DOI: https://doi.org/10.1097/YCO.0000000000000721
Hill JE, Harris C, Danielle L C, Boland P, Doherty AJ, Benedetto V, et al. The prevalence of mental health conditions in healthcare workers during and after a pandemic: Systematic review and meta-analysis. J Adv Nurs. 2022;78(6):1551-1573. doi: 10.1111/jan.15175. DOI: https://doi.org/10.1111/jan.15175
Li Y, Scherer N, Felix L, Kuper H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: A systematic review and meta-analysis. PLoS One. 2021;16(3):e0246454. doi: 10.1371/journal.pone.0246454. DOI: https://doi.org/10.1371/journal.pone.0246454
Chew NWS, Lee GKH, Tan BYQ, Jing M, Goh Y, Ngiam NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559-565. doi: 10.1016/j.bbi.2020.04.049. DOI: https://doi.org/10.1016/j.bbi.2020.04.049
Fried EI, Nesse RM. The impact of individual depressive symptoms on impairment of psychosocial functioning. PLoS One. 2014;9(2):e90311. doi: 10.1371/journal.pone.0090311. DOI: https://doi.org/10.1371/journal.pone.0090311
Levis B, Benedetti A, Thombs BD; DEPRESsion Screening Data (DEPRESSD) Collaboration. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. 2019;365:l1476. doi: 10.1136/bmj.l1476. DOI: https://doi.org/10.1136/bmj.l1476
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613. doi: 10.1046/j.1525-1497.2001.016009606.x. DOI: https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Arroll B, Goodyear-Smith F, Crengle S, Gunn J, Kerse N, Fishman T, et al. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann Fam Med. 2010;8(4):348-353. doi: 10.1370/afm.1139. DOI: https://doi.org/10.1370/afm.1139
Hassannia L, Taghizadeh F, Moosazadeh M, Zarghami M, Taghizadeh H, Dooki AF, et al. Anxiety and depression in health workers and general population during COVID-19 in IRAN: A cross-sectional study. Neuropsychopharmacol Rep. 2021;41(1):40-49. doi: 10.1002/npr2.12153. DOI: https://doi.org/10.1002/npr2.12153
Naser AY, Dahmash EZ, Al-Rousan R, Alwafi H, Alrawashdeh HM, Ghoul I, et al. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: A cross-sectional study. Brain Behav. 2020;10(8):e01730. doi: 10.1002/brb3.1730. DOI: https://doi.org/10.1002/brb3.1730
Rossi R, Socci V, Pacitti F, Di Lorenzo G, Di Marco A, Siracusano A, et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw Open. 2020;3(5):e2010185. doi: 10.1001/jamanetworkopen.2020.10185. DOI: https://doi.org/10.1001/jamanetworkopen.2020.10185
Zhu Z, Xu S, Wang H, Liu Z, Wu J, Li G, et al. COVID-19 in Wuhan: Sociodemographic characteristics and hospital support measures associated with the immediate psychological impact on healthcare workers. EClinicalMedicine. 2020;24:100443. doi: 10.1016/j.eclinm.2020.100443. DOI: https://doi.org/10.1016/j.eclinm.2020.100443
Fond G, Fernandes S, Lucas G, Greenberg N, Boyer L. Depression in healthcare workers: Results from the nationwide AMADEUS survey. Int J Nurs Stud. 2022;135:104328. doi: 10.1016/j.ijnurstu.2022.104328. DOI: https://doi.org/10.1016/j.ijnurstu.2022.104328
Ali S, Maguire S, Marks E, Doyle M, Sheehy C. Psychological impact of the COVID-19 pandemic on healthcare workers at acute hospital settings in the South-East of Ireland: an observational cohort multicentre study. BMJ Open. 2020;10(12):e042930. doi: 10.1136/bmjopen-2020-042930. DOI: https://doi.org/10.1136/bmjopen-2020-042930
Baker VB, Sowers CB, Hack NK. Lost productivity associated with headache and depression: a quality improvement project identifying a patient population at risk. J Headache Pain. 2020;21(1):50. doi: 10.1186/s10194-020-01107-4. DOI: https://doi.org/10.1186/s10194-020-01107-4
Patel RS, Bachu R, Adikey A, Malik M, Shah M. Factors related to physician burnout and its consequences: A review. Behav Sci (Basel). 2018;8(11):98. doi: 10.3390/bs8110098. DOI: https://doi.org/10.3390/bs8110098
Uz B, Savaşan E, Soğancı D. Anxiety, depression and burnout levels of Turkish healthcare workers at the end of the first period of COVID-19 pandemic in Turkey. Clin Psychopharmacol Neurosci. 2022;20(1):97-108. doi: 10.9758/cpn.2022.20.1.97. DOI: https://doi.org/10.9758/cpn.2022.20.1.97
Koksal E, Dost B, Terzi Ö, Ustun YB, Özdin S, Bilgin S. Evaluation of depression and anxiety levels and related factors among operating theater workers during the novel coronavirus (COVID-19) pandemic. J Perianesth Nurs. 2020;35(5):472-477. doi: 10.1016/j.jopan.2020.06.017. DOI: https://doi.org/10.1016/j.jopan.2020.06.017
Lee S, Hwang S, Kwon KT, Nam E, Chung US, Kim SW, et al. Prevalence and associated factors of depression and anxiety among healthcare workers during the coronavirus disease 2019 pandemic: A nationwide study in Korea. J Korean Med Sci. 2024;39(13):e120. doi: 10.3346/jkms.2024.39.e120. DOI: https://doi.org/10.3346/jkms.2024.39.e120
Slavich GM, Sacher J. Stress, sex hormones, inflammation, and major depressive disorder: Extending Social Signal Transduction Theory of Depression to account for sex differences in mood disorders. Psychopharmacology (Berl). 2019;236(10):3063-3079. doi: 10.1007/s00213-019-05326-9. DOI: https://doi.org/10.1007/s00213-019-05326-9
Matud MP, Díaz A, Bethencourt JM, Ibáñez I. Stress and psychological distress in emerging adulthood: A gender analysis. J Clin Med. 2020;9(9):2859. doi: 10.3390/jcm9092859. DOI: https://doi.org/10.3390/jcm9092859
Pengpid S, Peltzer K, Anantanasuwong D. Marital status, marital transition and health behaviour and mental health outcomes among middle-aged and older adults in Thailand: A national longitudinal study. Arch Gerontol Geriatr. 2024;117:105196. doi: 10.1016/j.archger.2023.105196. DOI: https://doi.org/10.1016/j.archger.2023.105196
Sotomayor-Beltran C, Matta-Solis H, Perez-Siguas R, Matta-Solis E, Matta-Zamudio L. Fear of COVID-19 among Peruvian people living in disadvantaged communities: A cross-sectional study. Clin Pract Epidemiol Ment Health. 2021;17:19-25. doi: 10.2174/1745017902117010019. PMID: 34040650; PMCID: PMC8097400... DOI: https://doi.org/10.2174/1745017902117010019
Bjelland I, Krokstad S, Mykletun A, Dahl AA, Tell GS, Tambs K. Does a higher educational level protect against anxiety and depression? The HUNT study. Soc Sci Med. 2008;66(6):1334-1345. doi: 10.1016/j.socscimed.2007.12.019. DOI: https://doi.org/10.1016/j.socscimed.2007.12.019
Zhang L, Wen J, Yuan L, Yan Y, Zhang Z, Li K, et al. Anxiety and depression in healthcare workers 2 years after COVID-19 infection and scale validation. Sci Rep. 2025;15(1):13893. doi: 10.1038/s41598-025-98515-w. DOI: https://doi.org/10.1038/s41598-025-98515-w
Serrano-Ripoll MJ, Meneses-Echavez JF, Ricci-Cabello I, Fraile-Navarro D, Fiol-deRoque MA, Pastor-Moreno G, et al. Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review and meta-analysis. J Affect Disord. 2020;277:347-357. doi: 10.1016/j.jad.2020.08.034. DOI: https://doi.org/10.1016/j.jad.2020.08.034
Mo Y, Deng L, Zhang L, Lang Q, Liao C, Wang N, et al. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J Nurs Manag. 2020;28(5):1002-1009. doi: 10.1111/jonm.13014. DOI: https://doi.org/10.1111/jonm.13014
Yassin A, Al-Mistarehi AH, Soudah O, Karasneh R, Al-Azzam S, Qarqash AA, et al. Trends of prevalence estimates and risk factors of depressive symptoms among healthcare workers over one year of the COVID-19 pandemic. Clin Pract Epidemiol Ment Health. 2022;18:e174501792206160. doi: 10.2174/17450179-v18-e2206160. DOI: https://doi.org/10.2174/17450179-v18-e2206160
Liu CH, Zhang E, Wong GTF, Hyun S, Hahm HC. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020;290:113172. doi: 10.1016/j.psychres.2020.113172. DOI: https://doi.org/10.1016/j.psychres.2020.113172
Ofori AA, Osarfo J, Agbeno EK, Manu DO, Amoah E. Psychological impact of COVID-19 on health workers in Ghana: A multicentre, cross-sectional study. SAGE Open Med. 2021;9:20503121211000919. doi: 10.1177/20503121211000919. DOI: https://doi.org/10.1177/20503121211000919
Emiral E, Bulut YE, Öztürk-Emiral G, Sarıca-Çevik H, Aksungur A. Psychosocial status of healthcare workers during the COVID-19 pandemic. Infect Dis Clin Microbiol. 2023;5(4):300-310. doi: 10.36519/idcm.2023.282. DOI: https://doi.org/10.36519//idcm.2023.282
Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020;88:901-907. doi: 10.1016/j.bbi.2020.05.026. DOI: https://doi.org/10.1016/j.bbi.2020.05.026
Smallwood N, Karimi L, Bismark M, Putland M, Johnson D, Dharmage SC, et al. High levels of psychosocial distress among Australian frontline healthcare workers during the COVID-19 pandemic: a cross-sectional survey. Gen Psychiatr. 2021;34(5):e100577. doi: 10.1136/gpsych-2021-100577. DOI: https://doi.org/10.1136/gpsych-2021-100577
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











