Patterns of Radiological Misinterpretation of Complete Anterior Cruciate Ligament Tears on Routine MRI Reports: An Arthroscopic Validation Study
DOI:
https://doi.org/10.54133/ajms.v10i1.2707Keywords:
Anterior cruciate ligament injuries, Arthroscopy, Diagnostic accuracy, Magnetic resonance imagingAbstract
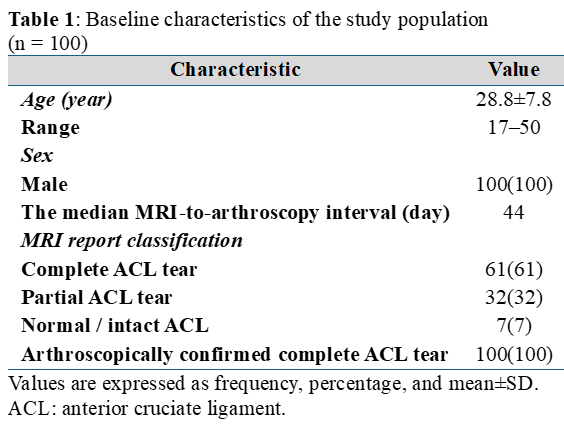
Background: Magnetic resonance imaging (MRI) is the primary noninvasive technique in the diagnosis of anterior cruciate ligament (ACL) injuries, and its performance is well described under ideal circumstances; however, the diagnostic accuracy in routine clinical practice is inadequately described. Objective: To determine the diagnostic accuracy of routine radiological MRI reports in the diagnosis of complete ACL tears when arthroscopy is used as the reference standard. Methods: This was a retrospective study, which involved 100 consecutive patients (28.8±7.8 years, and all males) who underwent knee arthroscopy with an intraoperative finding showing complete ACL tears. Preoperative MRI reports obtained from on-duty radiologists were reviewed and classified as complete, partial tear, or normal ACL. We calculated sensitivity for diagnosing complete tears in the ACL, and an exploratory analysis was done to examine the relationship between the MRI-arthroscopy interval and the accuracy of the diagnosis. Results: Routine MRI interpretation correctly detected complete ACL rupture in 61 cases with a sensitivity of 61.0% (95% CI: 51.2–70.0). It is significant to note that 32% of complete tears were underestimated as partial injuries, and 7% were misinterpreted as normal. The MRI-arthroscopy interval significantly influenced diagnostic outcomes (p=0.038); however, subgroup analyses were underpowered and remain hypothesis-generating. Conclusions: In routine clinical use, MRI interpretation achieved a suboptimal sensitivity (61%) in identifying arthroscopically proved complete ACL tears, and a significant proportion of cases were underestimated. To improve diagnostic accuracy, it is necessary to combine clinical examinations with imaging and employ radiologist-focused quality improvement programs.
Downloads
References
Sanders TL, Kremers HM, Bryan AJ, Larson DR, Dahm DL, Levy BA, et al. Incidence of anterior cruciate ligament tears and reconstruction. Am J Sports Med. 2016;44(6):1502–1507. doi: 10.1177/0363546516629944. DOI: https://doi.org/10.1177/0363546516629944
Martinez-Calderon J, Infante-Cano M, Matias-Soto J, Perez-Cabezas V, Galan-Mercant A, Garcia-Muñoz C. The Incidence of sport-related anterior cruciate ligament injuries: An overview of systematic reviews including 51 meta-analyses. J Funct Morphol Kinesiol. 2025;10(2):174. doi: 10.3390/jfmk10020174. DOI: https://doi.org/10.3390/jfmk10020174
Figueiredo P, Leitão R, Branco J, Pinheiro J. Anterior cruciate ligament injury: Risk factors and injury mechanisms: A systematic review. J Fam Med Prev Med. 2025;2(2):1–6. doi: 10.47363/jfmpm/2025(2)107. DOI: https://doi.org/10.47363/JFMPM/2025(2)107
Boden BP, Sheehan FT. Mechanism of non‐contact ACL injury: OREF Clinical Research Award 2021. J Orthopaed Res. 2021;40(3):531–540. doi: 10.1002/jor.25257. DOI: https://doi.org/10.1002/jor.25257
Allott NEH, Banger MS, McGregor AH. Evaluating the diagnostic pathway for acute ACL injuries in trauma centres: a systematic review. BMC Musculoskeletal Disord. 2022;23(1):649. doi: 10.1186/s12891-022-05595-0. DOI: https://doi.org/10.1186/s12891-022-05595-0
Huang Z, Cui J, Zhong M, Deng Z, Chen K, Zhu W. Risk factors of cartilage lesion after anterior cruciate ligament reconstruction. Front Cell Dev Biol. 2022; 10:935795. doi: 10.3389/fcell.2022.935795. DOI: https://doi.org/10.3389/fcell.2022.935795
Ali A. Evaluation of magnetic resonance imaging (MRI) versus knee arthroscopy in diagnosing anterior cruciate ligament (ACL) tears: A systematic review. Asian J Med Biomed. 2023;106–125. doi: 10.37231/ajmb.2023.1.s.669. DOI: https://doi.org/10.37231/ajmb.2023.1.S.669
Mohammad BA, Gharaibeh M. Magnetic resonance imaging of anterior cruciate ligament injury. Orthoped Res Rev. 2024; 16:233–242. doi: 10.2147/orr.s450336. DOI: https://doi.org/10.2147/ORR.S450336
Li K, Du J, Huang LX, Ni L, Liu T, Yang HL. The diagnostic accuracy of magnetic resonance imaging for anterior cruciate ligament injury in comparison to arthroscopy: A meta-analysis. Sci Rep. 2017;2;7(1):7583. doi: 10.1038/s41598-017-08133-4. DOI: https://doi.org/10.1038/s41598-017-08133-4
Phelan N, Rowland P, Galvin R, O’Byrne JM. A systematic review and meta-analysis of the diagnostic accuracy of MRI for suspected ACL and meniscal tears of the knee. Knee Surg Sports Traumatol Arthroscopy. 2015;24(5):1525–1539. doi: 10.1007/s00167-015-3861-8. DOI: https://doi.org/10.1007/s00167-015-3861-8
Krampla W, Roesel M, Svoboda K, Nachbagauer A, Gschwantler M, Hruby W. MRI of the knee: how do field strength and radiologist’s experience influence diagnostic accuracy and interobserver correlation in assessing chondral and meniscal lesions and the integrity of the anterior cruciate ligament? Eur Radiol. 2009;19(6):1519–1528. doi: 10.1007/s00330-009-1298-5. DOI: https://doi.org/10.1007/s00330-009-1298-5
Shantanu K, Singh S, Srivastava S, Saroj AK. The validation of clinical examination and MRI as a diagnostic tool for cruciate ligaments and meniscus injuries of the knee against diagnostic arthroscopy. Cureus. 2021;13(6):e15727. doi: 10.7759/cureus.15727. DOI: https://doi.org/10.7759/cureus.15727
Cohen JF, Korevaar DA, Altman DG, Bruns DE, Gatsonis CA, Hooft L, et al. STARD 2015 guidelines for reporting diagnostic accuracy studies: explanation and elaboration. BMJ Open. 2016;6(11):e012799. doi: 10.1136/bmjopen-2016-012799. DOI: https://doi.org/10.1136/bmjopen-2016-012799
Duc SR, Pfirrmann CWA, Koch PP, Zanetti M, Hodler J. Internal knee derangement assessed with 3-minute three-dimensional isovoxel true FISP MR sequence: Preliminary study. Radiology. 2008; 246(2):526–535. doi: 10.1148/radiol.2462062092. DOI: https://doi.org/10.1148/radiol.2462062092
Thomas S, Pullagura M, Robinson E, Cohen A, Banaszkiewicz P. The value of magnetic resonance imaging in our current management of ACL and meniscal injuries. Knee Surg Sports Traumatol Arthroscopy. 2007;15(5):533–536. doi: 10.1007/s00167-006-0259-7. DOI: https://doi.org/10.1007/s00167-006-0259-7
Yiannakopoulos CK, Vlastos IE, Sideri N, Papakonstantinou O. MRI and arthroscopic findings in acute and chronic ACL injuries. A pictorial essay. J Res Pract Musculoskeletal Syst. 2018;2(4):98–112. doi: 10.22540/jrpms-02-098. DOI: https://doi.org/10.22540/JRPMS-02-098
Challen J, Tang Y, Hazratwala K, Stuckey S. Accuracy of MRI diagnosis of internal derangement of the knee in a non‐specialized tertiary level referral teaching hospital. Australasian Radiol. 2007;51(5):426–431. doi: 10.1111/j.1440-1673.2007.01865.x. DOI: https://doi.org/10.1111/j.1440-1673.2007.01865.x
Navali AM, Bazavar M, Mohseni MA, Safari B, Tabrizi A. Arthroscopic evaluation of the accuracy of clinical examination versus MRI in diagnosing meniscus tears and cruciate ligament ruptures. Arch Iran Med. 2013;16(4):229-232. PMID: 23496367.
Zhang L, Wen X, Li JW, Jiang X, Yang XF, Li M. Diagnostic error and bias in the department of radiology: a pictorial essay. Insights Into Imaging. 2023;14(1):163. doi: 10.1186/s13244-023-01521-7. DOI: https://doi.org/10.1186/s13244-023-01521-7
Zhao M, Zhou Y, Chang J, Hu J, Liu H, Wang S, et al. The accuracy of MRI in the diagnosis of anterior cruciate ligament injury. Ann Transl Med. 2020;8(24):1657. doi: 10.21037/atm-20-7391. DOI: https://doi.org/10.21037/atm-20-7391
Tanaka S, Inoue Y, Masuda Y, Tian H, Jung H, Tanaka R. Diagnostic accuracy of physical examination tests for Suspected acute anterior cruciate ligament Injury: A systematic review and meta-analysis. Int J Sports Physical Ther. 2022;17(5):742–752. doi: 10.26603/001c.36434. DOI: https://doi.org/10.26603/001c.36434
Kohli A, Castillo S, Thakur U, Chhabra A. Structured reporting in musculoskeletal radiology. Semin Musculoskeletal Radiol. 2021;25(05):641-645. doi: 10.1055/s-0041-1736412. DOI: https://doi.org/10.1055/s-0041-1736412
Albano D, Dalili D, Huber FA, Snoj Z, Vieira A, Messina C. Current status of MSK radiology training: an international survey by the European Society of Musculoskeletal Radiology (ESSR) Young Club. Insights Into Imaging. 2021;12(1):126. doi: 10.1186/s13244-021-01070-x. DOI: https://doi.org/10.1186/s13244-021-01070-x
Altahawi F, Owens A, Caruso CH, Wetzel JR, Strnad GJ, Chiunda AB, et al. Development and operationalization of an automated workflow for correlation of knee MRI and arthroscopy findings. J Am Coll Radiol. 2023;21(4):609–616. doi: 10.1016/j.jacr.2023.04.010. DOI: https://doi.org/10.1016/j.jacr.2023.04.010
Wang DY, Liu SG, Ding J, Sun AL, Jiang D, Jiang J, et al. A deep learning model enhances clinicians’ diagnostic accuracy to more than 96% for anterior cruciate ligament ruptures on magnetic resonance imaging. Arthroscopy. 2023;40(4):1197–1205. doi: 10.1016/j.arthro.2023.08.010. DOI: https://doi.org/10.1016/j.arthro.2023.08.010
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2026 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











