Functional Outcomes after Posterior Cruciate Ligament Arthroscopic Reconstruction Surgery
DOI:
https://doi.org/10.54133/ajms.v8i1.1713Keywords:
Knee, Posterior cruciate ligament, Posterolateral corner, Posteromedial bundleAbstract
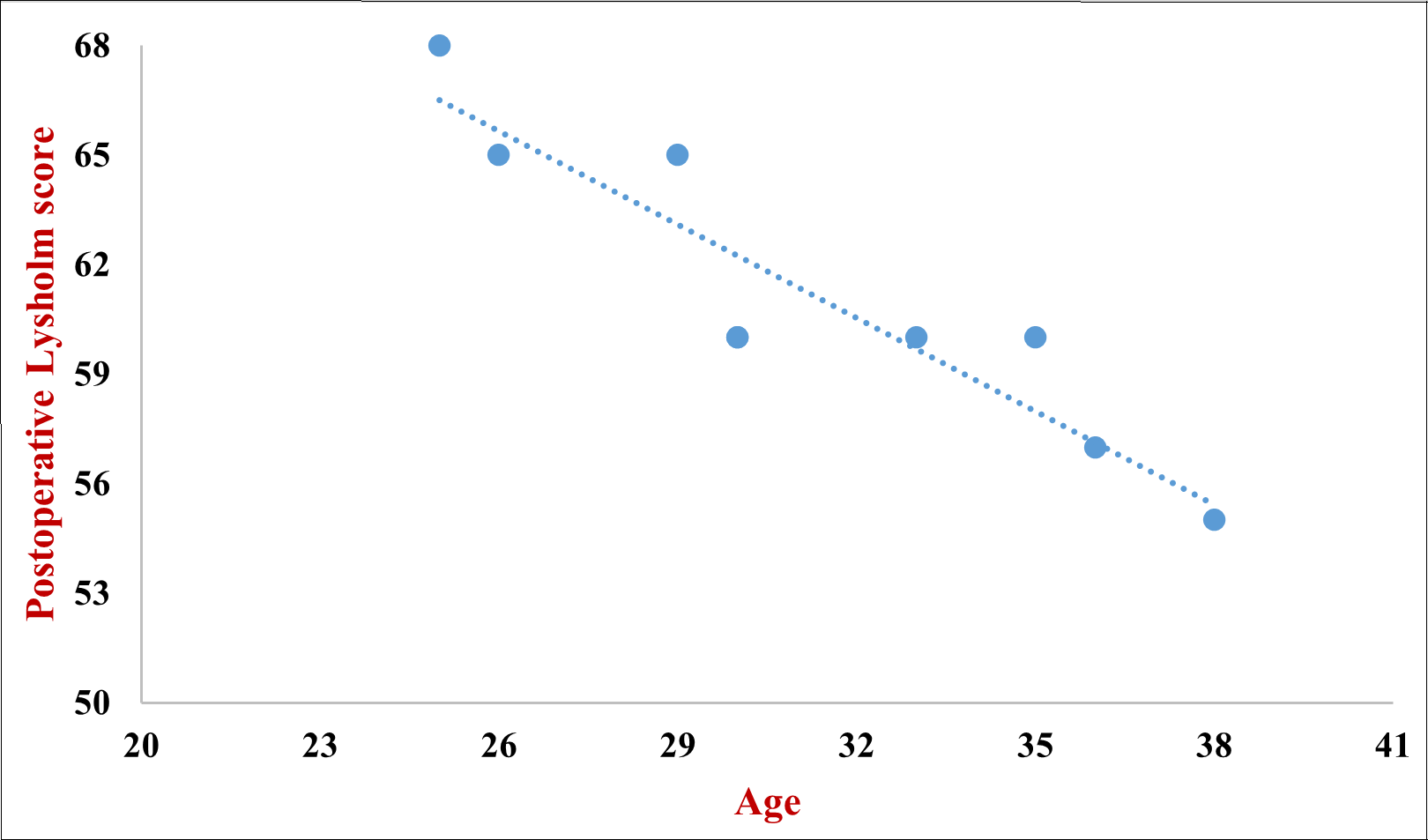
Background: The posterior cruciate ligament (PCL) primarily stabilizes the knee joint’s posterior part. PCL protects against tibial posterior translation and rotational instability by working together with the components of the posterolateral corner (PLC). PCL reconstruction has advancements; however, current approaches didn’t yield consistent results. Objective: To assess a functional outcome of patients after PCL reconstruction. Methods: A case series study was conducted from Jan 2021 till Jan 2022. We enrolled 10 participants with PCL injuries, ages between 25 and 36 years, late presentation more than 1 month, and excluded those with degenerative changes, multi-ligament injury, and limb malalignment. PCL reconstruction was performed. Knee arthroscopy was conducted to discover the PCL disfigurement. The Lysholm score was evaluated preoperatively and 6 months postoperatively. It ranges from 0 to 100 points. A score of 95-100 means excellent, 84-94 means good, 65-83 means fair, and 65 means poor. Results: The mean Lysholm score preoperatively was 60.7 and postoperatively was 89.4, with a significant difference. A significant correlation was found between age and Lysholm score after surgery, where younger age was associated with better functional outcomes. Conclusions: Age plays a role in the improvement of the Lysholm score postoperatively. The timing of PCLR surgery doesn’t affect the functional outcome when done for less than or more than six months.
Downloads
References
Pache S, Aman ZS, Kennedy M, Nakama GY, Moatshe G, Ziegler C, et al. Posterior cruciate ligament: Current concepts review. Arch Bone Jt Surg. 2018;6(1):8-18. PMID: 29430489.
Mygind-Klavsen B, Nielsen TG, Lind MC. Outcomes after posterior cruciate ligament (PCL) reconstruction in patients with isolated and combined PCL tears. Orthop J Sports Med. 2017;5(4):2325967117700077. doi: 10.1177/2325967117700077. DOI: https://doi.org/10.1177/2325967117700077
Jackson WF, van der Tempel WM, Salmon LJ, Williams HA, Pinczewski LA. Endoscopically-assisted single-bundle posterior cruciate ligament reconstruction: results at minimum ten-year follow-up. J Bone Joint Surg Br. 2008;90(10):1328-1333. doi: 10.1302/0301-620X.90B10.20517. DOI: https://doi.org/10.1302/0301-620X.90B10.20517
Brelin AM, Donohue MA, Balazs GC, LeClere LE, Rue JH, Dickens JF. Incidence and risk factors for reoperation following meniscal repair in a military population. J Surg Orthop Adv. 2018;27(1):47-51. PMID: 29762116. DOI: https://doi.org/10.3113/JSOA.2018.0047
Tucker CJ, Cotter EJ, Waterman BR, Kilcoyne KG, Cameron KL, Owens BD. Functional outcomes after isolated and combined posterior cruciate ligament reconstruction in a military population. Orthop J Sports Med. 2019;7(10):2325967119875139. doi: 10.1177/2325967119875139. DOI: https://doi.org/10.1177/2325967119875139
Kennedy NI, Wijdicks CA, Goldsmith MT, Michalski MP, Devitt BM, Årøen A, et al. Kinematic analysis of the posterior cruciate ligament, part 1: the individual and collective function of the anterolateral and posteromedial bundles. Am J Sports Med. 2013;41(12):2828-2838. doi: 10.1177/0363546513504287.
Anderson CJ, Ziegler CG, Wijdicks CA, Engebretsen L, LaPrade RF. Arthroscopically pertinent anatomy of the anterolateral and posteromedial bundles of the posterior cruciate ligament. J Bone Joint Surg Am. 2012;94(21):1936-1945. doi: 10.2106/JBJS.K.01710. DOI: https://doi.org/10.2106/JBJS.K.01710
Ahmad CS, Cohen ZA, Levine WN, Gardner TR, Ateshian GA, Mow VC. Codominance of the individual posterior cruciate ligament bundles. An analysis of bundle lengths and orientation. Am J Sports Med. 2003;31(2):221-225. doi: 10.1177/03635465030310021101. DOI: https://doi.org/10.1177/03635465030310021101
Kennedy NI, Wijdicks CA, Goldsmith MT, Michalski MP, Devitt BM, Årøen A, et al. Kinematic analysis of the posterior cruciate ligament, part 1: the individual and collective function of the anterolateral and posteromedial bundles. Am J Sports Med. 2013;41(12):2828-238. doi: 10.1177/0363546513504287. DOI: https://doi.org/10.1177/0363546513504287
Boutefnouchet T, Bentayeb M, Qadri Q, Ali S. Long-term outcomes following single-bundle transtibial arthroscopic posterior cruciate ligament reconstruction. Int Orthop. 2013;37(2):337-343. doi: 10.1007/s00264-012-1609-3. DOI: https://doi.org/10.1007/s00264-012-1609-3
Dennis MG, Fox JA, Alford JW, Hayden JK, Bach BR. Posterior cruciate ligament reconstruction- Current trends. J Knee Surg. 2004;17(03):133-139. doi: 10.1055/s-0030-1248211. DOI: https://doi.org/10.1055/s-0030-1248211
Shon OJ, Park JW, Kim BJ. Current concepts of posterolateral corner injuries of the knee. Knee Surg Relat Res. 2017;29(4):256-268. doi: 10.5792/ksrr.16.029.
Moulton SG, Cram TR, James EW, Dornan GJ, Kennedy NI, LaPrade RF. The supine internal rotation test: A pilot study evaluating tibial internal rotation in grade III posterior cruciate ligament tears. Orthop J Sports Med. 2015;3(2):2325967115572135. doi: 10.1177/2325967115572135. DOI: https://doi.org/10.1177/2325967115572135
Jung TM, Reinhardt C, Scheffler SU, Weiler A. Stress radiography to measure posterior cruciate ligament insufficiency: a comparison of five different techniques. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1116-1121. doi: 10.1007/s00167-006-0137-3. DOI: https://doi.org/10.1007/s00167-006-0137-3
Spiridonov SI, Slinkard NJ, LaPrade RF. Isolated and combined grade-III posterior cruciate ligament tears treated with double-bundle reconstruction with use of endoscopically placed femoral tunnels and grafts: operative technique and clinical outcomes. J Bone Joint Surg Am. 2011;93(19):1773-1780. doi: 10.2106/JBJS.J.01638. DOI: https://doi.org/10.2106/JBJS.J.01638
Jackman T, LaPrade RF, Pontinen T, Lender PA. Intraobserver and interobserver reliability of the kneeling technique of stress radiography for the evaluation of posterior knee laxity. Am J Sports Med. 2008;36(8):1571-1576. doi: 10.1177/0363546508315897. DOI: https://doi.org/10.1177/0363546508315897
Wilson KJ, Surowiec RK, Ho CP, Devitt BM, Fripp J, Smith WS, et al. Quantifiable imaging biomarkers for evaluation of the posterior cruciate ligament using 3-T magnetic resonance imaging: A feasibility study. Orthop J Sports Med. 2016;4(4):2325967116639044. doi: 10.1177/2325967116639044. DOI: https://doi.org/10.1177/2325967116639044
Chahla J, von Bormann R, Engebretsen L, LaPrade RF. Anatomic posterior cruciate ligament reconstruction: State of the art. JISAKOS. 2016;1(5):292-302. Available from: https://www.jisakos.com/article/S2059-7754(21)00174-7/fulltext DOI: https://doi.org/10.1136/jisakos-2016-000078
LaPrade RF, Heikes C, Bakker AJ, Jakobsen RB. The reproducibility and repeatability of varus stress radiographs in the assessment of isolated fibular collateral ligament and grade-III posterolateral knee injuries. An in vitro biomechanical study. J Bone Joint Surg Am. 2008;90(10):2069-2076. doi: 10.2106/JBJS.G.00979. DOI: https://doi.org/10.2106/JBJS.G.00979
Laprade RF, Bernhardson AS, Griffith CJ, Macalena JA, Wijdicks CA. Correlation of valgus stress radiographs with medial knee ligament injuries: an in vitro biomechanical study. Am J Sports Med. 2010;38(2):330-338. doi: 10.1177/0363546509349347. DOI: https://doi.org/10.1177/0363546509349347
Shelbourne KD, Muthukaruppan Y. Subjective results of nonoperatively treated, acute, isolated posterior cruciate ligament injuries. Arthroscopy. 2005;21(4):457-461. doi: 10.1016/j.arthro.2004.11.013. DOI: https://doi.org/10.1016/j.arthro.2004.11.013
Gill TJ, DeFrate LE, Wang C, Carey CT, Zayontz S, Zarins B, et al. The effect of posterior cruciate ligament reconstruction on patellofemoral contact pressures in the knee joint under simulated muscle loads. Am J Sports Med. 2004;32(1):109-115. doi: 10.1177/0095399703258794. DOI: https://doi.org/10.1177/0095399703258794
Hermans S, Corten K, Bellemans J. Long-term results of isolated anterolateral bundle reconstructions of the posterior cruciate ligament: a 6- to 12-year follow-up study. Am J Sports Med. 2009;37(8):1499-1507. doi: 10.1177/0363546509333479. DOI: https://doi.org/10.1177/0363546509333479
Kim SJ, Jung M, Moon HK, Kim SG, Chun YM. Anterolateral transtibial posterior cruciate ligament reconstruction combined with anatomical reconstruction of posterolateral corner insufficiency: comparison of single-bundle versus double-bundle posterior cruciate ligament reconstruction over a 2- to 6-year follow-up. Am J Sports Med. 2011;39(3):481-489. doi: 10.1177/0363546510385398. DOI: https://doi.org/10.1177/0363546510385398
Chahla J, Moatshe G, Cinque ME, Dornan GJ, Mitchell JJ, Ridley TJ, et al. Single-bundle and double-bundle posterior cruciate ligament reconstructions: A systematic review and meta-analysis of 441 patients at a minimum 2 years' follow-up. Arthroscopy. 2017;33(11):2066-2080. doi: 10.1016/j.arthro.2017.06.049. DOI: https://doi.org/10.1016/j.arthro.2017.06.049
Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10(3):150-154. doi: 10.1177/036354658201000306. DOI: https://doi.org/10.1177/036354658201000306
Ng JW, Ahmad AR, Solayar GN. Functional outcomes following posterior cruciate ligament and posterolateral corner reconstructions. A three-year experience in Seremban, Malaysia. Malays Orthop J. 2020;14(2):90-93. doi: 10.5704/MOJ.2007.017. DOI: https://doi.org/10.5704/MOJ.2007.017
Caldas MTL, Braga GF, Mendes SL, da Silveira JM, Kopke RM. Posterior cruciate ligament injury: characteristics and associations of most frequent injuries. Rev Bras Ortop. 2013;48(5):427-431. doi: 10.1016/j.rboe.2012.09.010. DOI: https://doi.org/10.1016/j.rboe.2012.09.010
Schulz MS, Russe K, Weiler A, Eichhorn HJ, Strobel MJ. Epidemiology of posterior cruciate ligament injuries. Arch Orthop Trauma Surg. 2003;123(4):186-191. doi: 10.1007/s00402-002-0471-y. DOI: https://doi.org/10.1007/s00402-002-0471-y
Bernhardson AS, DePhillipo NN, Daney BT, Kennedy MI, Aman ZS, LaPrade RF. Posterior tibial slope and risk of posterior cruciate ligament injury. Am J Sports Med. 2019;47(2):312-317. doi: 10.1177/0363546518819176. DOI: https://doi.org/10.1177/0363546518819176
Hohmann E, Glatt V, Tetsworth K. Early or delayed reconstruction in multi-ligament knee injuries: A systematic review and meta-analysis. Knee. 2017;24(5):909-916. doi: 10.1016/j.knee.2017.06.011. DOI: https://doi.org/10.1016/j.knee.2017.06.011
Rusdi A, Shahrulazua A, Siti HT, Nizlan NM. Short-term functional outcomes of a delayed single-stage reconstruction of chronic posterior cruciate ligament and posterolateral corner deficiency. Clin Ter. 2014;165(1):e28-34. doi: 10.7471/CT.2014.1668.
Shon OJ, Park JW, Kim BJ. Current concepts of posterolateral corner injuries of the knee. Knee Surg Relat Res. 2017;29(4):256-268. doi: 10.5792/ksrr.16.029. DOI: https://doi.org/10.5792/ksrr.16.029
Cury RP, Castro Filho RN, Sadatsune DA, do Prado DR, Gonçalves RJ, Mestriner MB. Double-bundle PCL reconstruction using autologous hamstring tendons: outcome with a minimum 2-year follow-up. Rev Bras Ortop. 2017;52(2):203-209. doi: 10.1016/j.rboe.2017.02.006. DOI: https://doi.org/10.1016/j.rboe.2017.02.006
Petrillo S, Volpi P, Papalia R, Maffulli N, Denaro V. Management of combined injuries of the posterior cruciate ligament and posterolateral corner of the knee: a systematic review. Br Med Bull. 2017;123(1):47-57. doi: 10.1093/bmb/ldx014. DOI: https://doi.org/10.1093/bmb/ldx014
Kim SJ, Lee SK, Kim SH, Kim SH, Jung M. Clinical outcomes for reconstruction of the posterolateral corner and posterior cruciate ligament in injuries with mild grade 2 or less posterior translation: comparison with isolated posterolateral corner reconstruction. Am J Sports Med. 2013;41(7):1613-1620. doi: 10.1177/0363546513485927. DOI: https://doi.org/10.1177/0363546513485927
Lind M, Nielsen TG, Behrndtz K. Both isolated and multi-ligament posterior cruciate ligament reconstruction results in improved subjective outcome: results from the Danish Knee Ligament Reconstruction Registry. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1190-1196. doi: 10.1007/s00167-017-4577-8. DOI: https://doi.org/10.1007/s00167-017-4577-8
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











