Accuracy of Endocavitary and Transperineal Ultrasound in Evaluating Fistula-in-Ano
DOI:
https://doi.org/10.54133/ajms.v10i1.2643Keywords:
Diagnostic accuracy, Endocavitary ultrasound, Fistula in ano, MRI, Parks classification , Transperineal ultrasoundAbstract
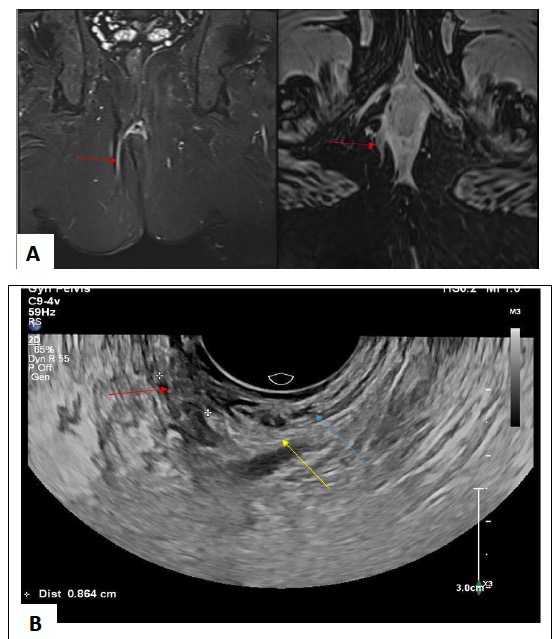
Background: Fistula-in-ano is an abnormal connection between the anal canal and the skin of the perineum, affecting 1.7-2.3/10,000 persons/year. Appropriate evaluations and imaging are necessary to decrease recurrence rate. Objective: Determining accuracy of endocavitary and transperineal ultrasound relative to magnetic resonance imaging in evaluation of perianal fistulas. Methods: A cross-sectional study was conducted on 40 patients with perianal fistula. Endocavitary, transperineal ultrasound and magnetic resonance imaging (MRI) were done for all patients. Many variables were recorded, including location, number of tracts, their relation to the anal sphincters (course), internal opening, external openings, length of tract, distances from the anal verge, and any associated abscess or side branching. Results: Of the 40 patients studied, both modalities showed compatibility between US and MRI for location of fistula, nearly perfect for opening to skin and opening to anal mucosa, and substantial for course of fistula, association collection, and side branching. For fistula length, the analysis revealed a statistically significant mean bias of 4.575 (p<0.001), indicating that MRI measurement is higher than US. For distance from anal verge bias, it is 2.575 (p<0.001), with the MRI measurement being higher than the US. Conclusions: Ultrasonography is a reliable, cost-effective alternative to MRI for assessing fistula in ano. Although MRI may still be preferred for more complex cases, ultrasound demonstrated high agreement in evaluating location, opening positions, course of fistula, and associated anatomical features.
Downloads
References
Varsamis N, Kosmidis C, Chatzimavroudis G, Sapalidis K, Efthymiadis C, Kiouti FA, et al. Perianal fistulas: A review with emphasis on preoperative imaging. Adv Med Sci. 2022;67(1):114-122. doi: 10.1016/j.advms.2022.01.002. DOI: https://doi.org/10.1016/j.advms.2022.01.002
Li J, Chen SN, Lin YY, Zhu ZM, Ye DL, Chen F, et a. Diagnostic accuracy of three-dimensional endoanal ultrasound for anal fistula: A systematic review and meta-analysis. Turk J Gastroenterol. 2021;32(11):913-922. doi: 10.5152/tjg.2021.20750. DOI: https://doi.org/10.37766/inplasy2020.7.0090
Jawad AM, Kadhim MA, Al-Jobouri ZK, Hussain MAA. The value of magnetic resonance imaging in the evaluation of peri-anal fistula. Iraqi J Med Sci. 2018;16(2):166-176. doi: 10.22578/IJMS.16.2.8. DOI: https://doi.org/10.22578/IJMS.16.2.8
Ren J, Bai W, Gu L, Li X, Peng X, Li W. Three-dimensional pelvic ultrasound is a practical tool for the assessment of anal fistula. BMC Gastroenterol. 2023;23(1):134. doi: 10.1186/s12876-023-02715-5. DOI: https://doi.org/10.1186/s12876-023-02715-5
Singh K, Singh N, Thukral C, Singh KP, Bhalla V. Magnetic resonance imaging (MRI) evaluation of perianal fistulae with surgical correlation. J Clin Diagn Res. 2014;8(6):RC01-RC4. doi: 10.7860/JCDR/2014/7328.4417. DOI: https://doi.org/10.7860/JCDR/2014/7328.4417
Siddiqui MR, Ashrafian H, Tozer P, Daulatzai N, Burling D, Hart A, et al. A diagnostic accuracy meta-analysis of endoanal ultrasound and MRI for perianal fistula assessment. Dis Colon Rectum. 2012;55(5):576-585. doi: 10.1097/DCR.0b013e318249d26c. DOI: https://doi.org/10.1097/DCR.0b013e318249d26c
Meegada SR, Alapati KV, Varughese M. (2024). Importance of high-frequency and low-frequency three-dimensional endoanal ultrasound scan in diagnosing perianal fistula and abscess. Int Surg J. 2024;11(6):908–917. doi: 10.18203/2349-2902.isj20241389. DOI: https://doi.org/10.18203/2349-2902.isj20241389
Akhoundi N, Bozchelouei JK, Abrishami A, Frootan M, Siami A, Alimadadi E, et al. Comparison of MRI and endoanal ultrasound in assessing intersphincteric, transsphincteric, and suprasphincteric perianal fistula. J Ultrasound Med. 2023;42(9):2057-2064. doi: 10.1002/jum.16225. DOI: https://doi.org/10.1002/jum.16225
Alshoabi SA, Binnuhaid AA, Hamid AM, Alhazmi FH, Qurashi AA, Gareeballah A, et al. Ultrasound assessment of low type intersphincteric perianal fistulas in Yemen. Sci Rep. 2025;15(1):22117. doi: 10.1038/s41598-025-06284-3. DOI: https://doi.org/10.1038/s41598-025-06284-3
Tabry H, Farrands PA. Update on anal fistulae: surgical perspectives for the gastroenterologist. Can J Gastroenterol. 2011;25(12):675-680. doi: 10.1155/2011/931316. DOI: https://doi.org/10.1155/2011/931316
Arkenbosch JHC, van Ruler O, de Vries AC, van der Woude CJ, Dwarkasing RS. The role of MRI in perianal fistulizing disease: diagnostic imaging and classification systems to monitor disease activity. Abdom Radiol (NY). 2025;50(2):589-597. doi: 10.1007/s00261-024-04455-w. DOI: https://doi.org/10.1007/s00261-024-04455-w
Felt-Bersma RJ. Endoanal ultrasound in perianal fistulas and abscesses. Dig Liver Dis. 2006;38(8):537-543. doi: 10.1016/j.dld.2006.02.016. DOI: https://doi.org/10.1016/j.dld.2006.02.016
Domkundwar SV, Shinagare AB. Role of transcutaneous perianal ultrasonography in evaluation of fistulas in ano. J Ultrasound Med. 2007;26(1):29-36. doi: 10.7863/jum.2007.26.1.29. DOI: https://doi.org/10.7863/jum.2007.26.1.29
Roman Boles MS, Awadallah MY, Shawali HAS. Farag A, El-Sayed RF. Role of transperineal ultrasound in evaluation of patients with perianal inflammatory disorders. Egypt J Radiol Nucl Med. 2022;53:141. doi: 10.1186/s43055-022-00812-1. DOI: https://doi.org/10.1186/s43055-022-00812-1
Schwartz DA, Wiersema MJ, Dudiak KM, Fletcher JG, Clain JE, Tremaine WJ, et al. A comparison of endoscopic ultrasound, magnetic resonance imaging, and exam under anesthesia for evaluation of Crohn's perianal fistulas. Gastroenterology. 2001;121(5):1064-1072. doi: 10.1053/gast.2001.28676. DOI: https://doi.org/10.1053/gast.2001.28676
Mallouhi A, Bonatti H, Peer S, Lugger P, Conrad F, Bodner G. Detection and characterization of perianal inflammatory disease: accuracy of transperineal combined gray scale and color Doppler sonography. J Ultrasound Med. 2004;23(1):19-27. doi: 10.7863/jum.2004.23.1.19. DOI: https://doi.org/10.7863/jum.2004.23.1.19
Sudoł-Szopińska I, Kucharczyk A, Kołodziejczak M, Warczyńska A, Pracoń G, Wiączek A. Comparison of endosonography and magnetic resonance imaging in the diagnosis of high anal fistulas. J Ultrason. 2014;14(57):142–151. doi: 10.15557/JoU.2014.0014. DOI: https://doi.org/10.15557/JoU.2014.0014
Mashhour AN, Omar HS, Marzouk AS, Raslan MM, Farag A. Evaluation of the role of endoanal ultrasonography in preoperative assessment of perianal fistula. Egypt J Surg. 2015;34(2). doi: 10.4103/1110-1121.155723. DOI: https://doi.org/10.4103/1110-1121.155723
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2026 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











