Construction of an Atopic Symptom Questionnaire and Evaluation of Peri-menstrual Atopy in Women of Reproductive Age
DOI:
https://doi.org/10.54133/ajms.v9i1.2286Keywords:
Atopic Symptoms, Menstrual phases, Perimenstrual atopy, Reproductive-age femaleAbstract
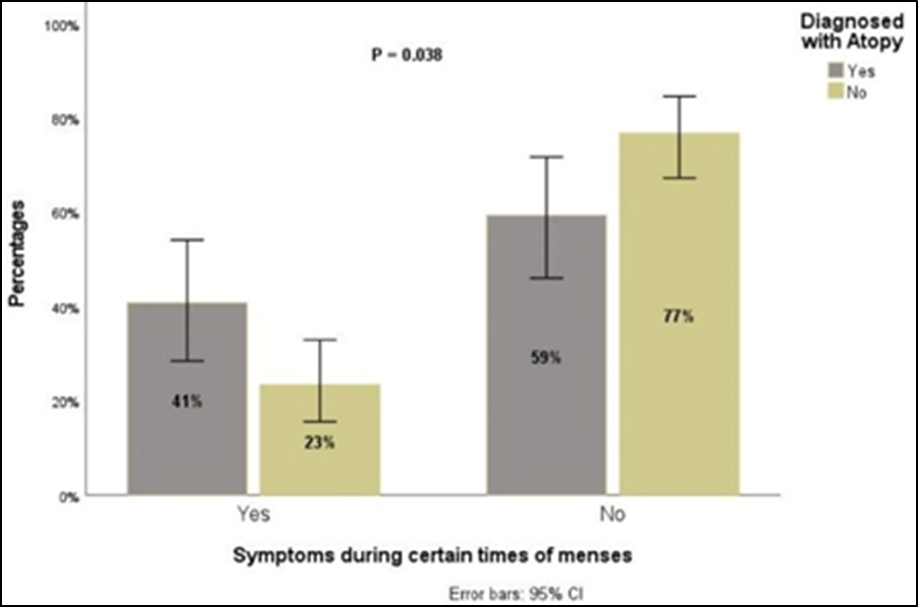
Background: Atopic disorders, such as asthma, atopic dermatitis (AD), and allergic rhinitis (AR), are rising globally. In reproductive-age women, hormonal fluctuations during the menstrual cycle can trigger or worsen symptoms, a condition termed perimenstrual atopy (PMA). Despite its prevalence, PMA remains under-recognized, especially in healthy females, and no standardized tool exists for its comprehensive assessment. Objective: To determine PMA occurrence in females with and without diagnosed atopy and to develop and validate the Atopic Symptom Score Questionnaire (ASQ) for PMA evaluation. Methods: This observational study included 145 reproductive-age females (54 atopic, 91 non-atopic) with regular menstrual cycles. The ASQ was constructed by integrating validated tools for asthma, AD, and AR. Content validity was confirmed by experts, and internal reliability was strong. After pilot testing, the finalized ASQ was administered via face-to-face interviews. Participants rated symptom severity and indicated the timing of symptom onset in relation to menstrual phases. Mean ASQ scores and the frequency of PMA were analyzed, and the comparison between atopic and non-atopic groups was conducted. Results: PMA was reported in 29.9% of participants, more often in atopic (40.7%) than non-atopic females (23.3%). The most common symptoms were breathlessness, throat discomfort, and nasal congestion. ASQ scores were significantly higher in atopic individuals (11.5 vs. 2.41, p<0.001), with most exacerbations during menstrual and premenstrual phases. Conclusions: The ASQ is a valid tool for assessing PMA. PMA is common and underdiagnosed, even among non-atopic females, highlighting the need for greater clinical awareness and standardized evaluation.
Downloads
References
Thomsen SF. Epidemiology and natural history of atopic diseases. Eur Clin Respir J. 2015;2(1):24642. doi: 10.3402/ecrj.v2.24642. DOI: https://doi.org/10.3402/ecrj.v2.24642
Golden DBK, Wang J, Waserman S, Akin C, Campbell RA, Ellis AK, et al. Anaphylaxis: A 2023 practice parameter update. Ann Allergy Asma Immunol. 2024;132(2):124-176. doi: 10.10/j.anal.2023.09.015. DOI: https://doi.org/10.1016/j.anai.2023.09.015
Johansson SG, Bieber T, Dahl R, Friedmann PS, Lanier BQ, Lockey RF, et al. Revised nomenclature for allergy for global use: Report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol. 2004;113(5):832-836. doi: 10.1016/j.jaci.2003.12.591. DOI: https://doi.org/10.1016/j.jaci.2003.12.591
Ring J. Terminology of allergic phenomena. Chem Immunol Allergy. 2014;69(1):46–52. doi:10.1159/000358500. DOI: https://doi.org/10.1159/000358500
Ring J, Przybilla B, Ruzicka T, editors, Handbook of Atopic Eczema. Berlin, Heidelberg: Springer Berlin Heidelberg; 2006. doi: 10.1007/3-540-29856-8. DOI: https://doi.org/10.1007/3-540-29856-8
Engler-Chiurazzi EB, Chastain WH, Citron KK, Lambert LE, Kikkeri DN, Shrestha SS. Estrogen, the peripheral immune system and major depression – a reproductive lifespan perspective. Front Behav Neurosci. 2022;16. doi: 10.3389/fnbeh.2022.850623. DOI: https://doi.org/10.3389/fnbeh.2022.850623
Kirmaz C, Yuksel H, Mete N, Bayrak P, Baytur YB. Is the menstrual cycle affecting the skin prick test reactivity? Asian Pac J Allergy Immunol. 2004;22(4):197–203. PMID: 15783132.
Murakami K, Sawada A, Mori T, Sakuyama S, Tokudome Y. Effect of estrogen/progesterone ratio on the differentiation and the barrier function of epidermal keratinocyte and three-dimensional cultured human epidermis. Life Sci. 2022;293:120356. doi: 10.1016/j.lfs.2022.120356. DOI: https://doi.org/10.1016/j.lfs.2022.120356
Graziottin A, Serafini A. Perimenstrual asthma: from pathophysiology to treatment strategies. Multidiscip Respir Med. 2016;11(1):30. doi: 10.1186/s40248-016-0065-0. DOI: https://doi.org/10.1186/s40248-016-0065-0
Weare-Regales N, Chiarella SE, Cardet JC, Prakash YS, Lockey RF. Hormonal effects on asthma, rhinitis, and eczema. J Allergy Clin Immunol Pract. 2022;10(8):2066–2073. doi: 10.1016/j.jaip.2022.04.002. DOI: https://doi.org/10.1016/j.jaip.2022.04.002
Haeggström A, Östberg B, Stjerna P, Graf P, Hallén H. Nasal mucosal swelling and reactivity during a menstrual cycle. ORL. 2000;62(1):39–42. doi: 10.1159/000027713. DOI: https://doi.org/10.1159/000027713
Vrieze A, Postma DS, Kerstjens HAM. Perimenstrual asthma: a syndrome without known cause or cure. J Allergy Clin Immunol. 2003;112(2):271–282. doi: 10.1067/mai.2003.1676. DOI: https://doi.org/10.1067/mai.2003.1676
Farha S, Asosingh K, Laskowski D, Hammel J, Dweik RA, Wiedemann HP, et al. Effects of the menstrual cycle on lung function variables in women with asthma. Am J Respir Crit Care Med. 2009;180(4):304–310. doi: 10.1164/rccm.200904-0497OC. DOI: https://doi.org/10.1164/rccm.200904-0497OC
Chhabra SK, Chhabra P. Gender differences in perception of dyspnea, assessment of control, and quality of life in asthma. J Asthma, 2011;48(6):609–615. doi: 10.3109/02770903.2011.587577. DOI: https://doi.org/10.3109/02770903.2011.587577
Frank RT. The hormonal causes of premenstrual tension. Arch Neurol Psychiatry. 1931;26(5):1053. doi: 10.1001/archneurpsyc.1931.02230110151009. DOI: https://doi.org/10.1001/archneurpsyc.1931.02230110151009
Aissani S, Ararem I, Haouichat H, Haffaf M, Zitouni A. Clinical and spirometric characteristics of premenstrual asthma. Int J of Allergy Medications. 2019;5(1). doi: 10.23937/2572-3308.1510041. DOI: https://doi.org/10.23937/2572-3308.1510041
Murphy VE, Gibson PG. Premenstrual asthma: prevalence, cycle-to-cycle variability and relationship to oral contraceptive use and menstrual symptoms. J ORLAsthma. 2008;45(8):696–704. doi: 10.1080/02770900802207279. DOI: https://doi.org/10.1080/02770900802207279
Wood PR, Smith B, O'Donnell L, Forkner E, Lara M, Peters JI. Quantifying asthma symptoms in adults: the Lara asthma symptom scale. J Allergy Clin Immunol. 2007;120(6):1368–1372. doi: 10.1016/j.jaci.2007.09.025. DOI: https://doi.org/10.1016/j.jaci.2007.09.025
American Thoracic Society. Asthma Control Questionnaire (ACQ). [Internet]. American Thoracic Society; [cited 2025 Jul 12]. Available from: https://www.thoracic.org/members/assemblies/assemblies/srn/questionaires/acq.php
DermNet New Zealand. EASI score. [Internet]. DermNet New Zealand; [cited 2025 Jul 12]. Available from: https://dermnetnz.org/topics/easi-score
Oakley A. SCORAD index. [Internet]. Hamilton, New Zealand: DermNet New Zealand; 2009 [cited 2025 Jul 12]. Available from: https://dermnetnz.org/topics/scorad
Charman CR, Venn AJ, Ravenscroft JC, Williams HC. Translating patient‐oriented eczema measure scores into clinical practice by suggesting severity strata derived using anchor‐based methods. Br J Dermatol. 2013;169(6):1326–1332. doi: 10.1111/bjd.12590. DOI: https://doi.org/10.1111/bjd.12590
Ontosight AI. Total nasal symptom score (TNSS). [Internet]. Ontosight AI; [cited 2025 Jul 12]. Available from: https://ontosight.ai/glossary/term/Total-Nasal-Symptom-Score---TNSS
Ellis AK, Soliman M, Steacy L, Boulay MÈ, Boulet LP, Keith PK, et al. The Allergic Rhinitis – Clinical Investigator Collaborative (AR-CIC): nasal allergen challenge protocol optimization for studying AR pathophysiology and evaluating novel therapies. J Allergy Clin Immunol. 2015;135(4):888–894. doi: 10.1186/s13223-015-0082-0. DOI: https://doi.org/10.1016/j.jaci.2014.12.1121
Skobeloff EM, Spivey WH, Silverman R, Eskin BA, Harchelroad F, Alessi TV. The effect of the menstrual cycle on asthma presentations in the emergency department. Arch Intern Med. 1996;156(16):1837–1840. PMID: 8790078. DOI: https://doi.org/10.1001/archinte.1996.00440150091010
Brenner BE, Holmes TM, Mazal B, Camargo CA Jr. Relation between phase of the menstrual cycle and asthma presentations in the emergency department. Thorax. 2005;60(10):806–809. doi: 10.1136/thx.2004.033928. DOI: https://doi.org/10.1136/thx.2004.033928
Eliasson O, Scherzer HH, DeGraff AC. Morbidity in asthma in relation to the menstrual cycle. J Allergy Clin Immunol. 1986;77(1 Pt 1):87–94. doi: 10.1016/0091-6749(86)90328-3. DOI: https://doi.org/10.1016/0091-6749(86)90328-3
Suzuki K, Hasegawa T, Sakagami T, Koya T, Toyabe S, Akazawa K, et al. Analysis of perimenstrual asthma based on questionnaire surveys in Japan. Allergol Int. 2007;56(3):249–255. doi: 10.2332/allergolint.O-06-475. DOI: https://doi.org/10.2332/allergolint.O-06-475
Mosbeh A, Abdelrahman RM. The impact of pregnancy and phases of the menstrual cycle on atopic dermatitis. Austin J Dermatol. 2017;4(3):1081.
Cho S, Kim HJ, Oh SH, Park CO, Jung JY, Lee KH. The influence of pregnancy and menstruation on the deterioration of atopic dermatitis symptoms. Ann Dermatol. 2010;22(2):180. doi: 10.5021/ad.2010.22.2.180. DOI: https://doi.org/10.5021/ad.2010.22.2.180
Grajczyk A, Sobczyk K, Dżaman K. Nasal and Eustachian tube function during menstrual cycle. Otolaryngol Pol. 2025;79(3):1–8. doi: 10.5604/01.3001.0055.0197. DOI: https://doi.org/10.5604/01.3001.0055.0197
Stübner UP, Gruber D, Berger UE, Toth J, Marks B, Huber J, et al. The influence of female sex hormones on nasal reactivity in seasonal allergic rhinitis. Allergy. 1999;54(8):865–871. doi: 10.1034/j.1398-9995.1999.00961.x. DOI: https://doi.org/10.1034/j.1398-9995.1999.00961.x
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











