Analysis of Complete Blood Count-Derived Inflammatory Biomarkers in Patients Underwent Total Knee Arthroplasty: A Retrospective Study
DOI:
https://doi.org/10.54133/ajms.v8i1.1711Keywords:
Biomarkers, Blood transfusion, Complete blood count, Correlation, Post-operative analgesic, Total knee arthroplastyAbstract
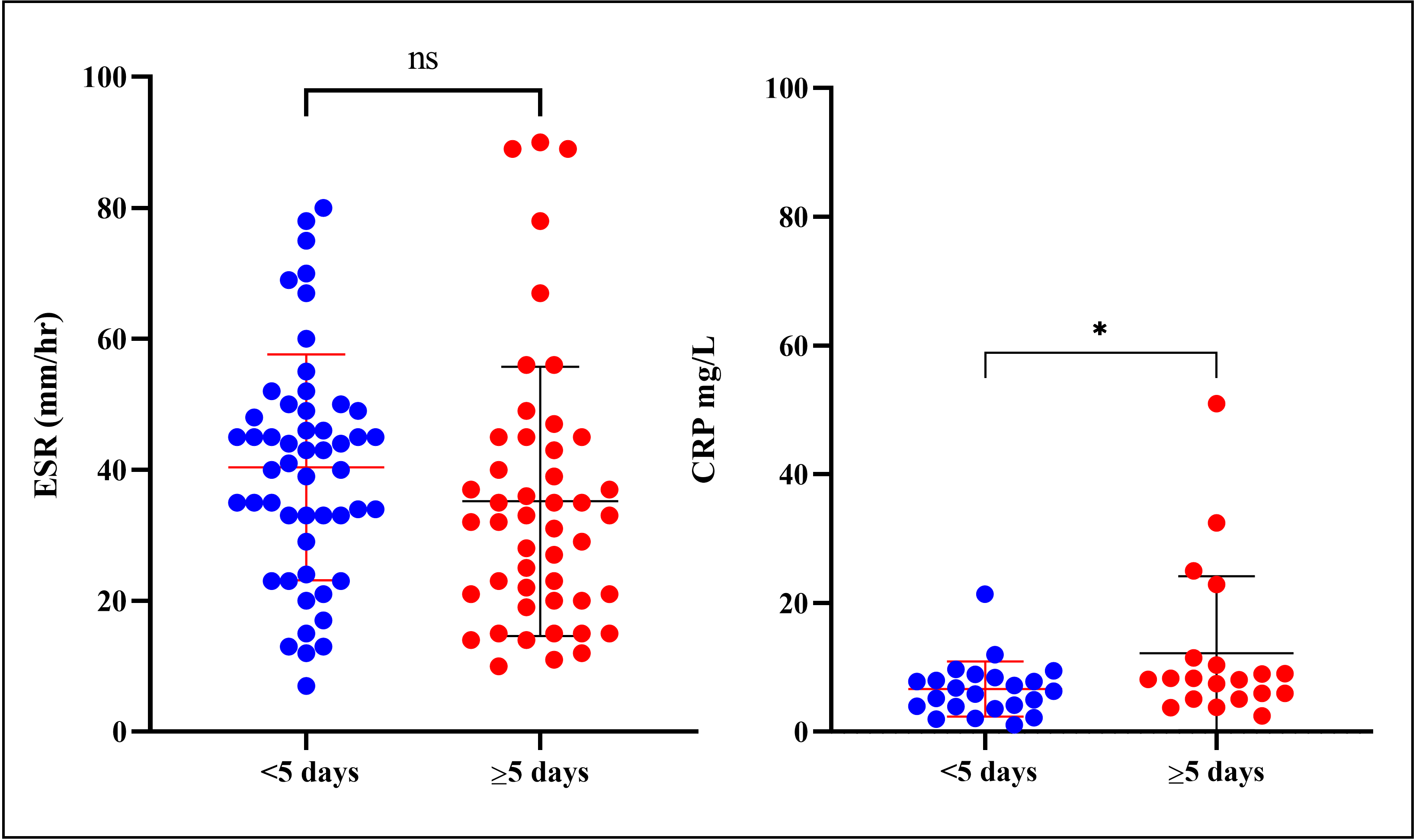
Background: Pain, bleeding, and anemia are frequent complications of total knee arthroplasty (TKA). Objective: To analyze CBC-derived biomarkers in patients who underwent TKA to predict postoperative complications. Methods: This retrospective study evaluated neutrophil-lymphocyte ratio (NLR), platelet-lymphocyte ratio (PLR), monocyte-to-lymphocyte ratio (MLR), platelet-monocyte ratio (PMR), hemoglobin-platelet ratio (HPR), hemoglobin-lymphocyte ratio (HLR). Results: A total of 99 patients’ records were investigated; their average age was 64.57±8.4. Significant differences in NLR and HLR were noted between the patients who needed <5 days and ≥ 5 days of opioid analgesic (OPA). Hence, the patients with higher NLR and HLR needed longer OPA (≥ 5 days) than the patients with lower NLR and HLR. Likewise, NLR, MLR, PLR, and HLR were significantly higher in the patients who needed longer non-OPA (>20 days). Additionally, the duration of non-OPA usage had a significantly high positive correlation (r= 0.967, p<0.0001) with NLR, and a moderate positive correlation with PLR (r=0.535, p<0.0001) and HLR (r= 0.6216, p<0.0001). On the other hand, the pre-operative NLR, MLR, PLR, and HLR of the patients who needed blood transfusion ≥ 1.0 pint (0.47 L) was significantly higher than those who did not need blood transfusion. Blood transfusion showed a significantly positive correlation (r=0.8419, p<0.0001) with NLR; also, there was a moderate positive correlation with PLR (r=0.5257, p<0.0001) and HLR (r=0.5841, p<0.0001). Conclusions: CBC-derived biomarkers can be utilized for predicting the duration and need for postoperative analgesics and blood transfusion.
Downloads
References
Yu H, Huang T, Lu WW, Tong L, Chen D. Osteoarthritis pain. Int J Mol Sci. 2022;23(9):4642. doi: 10.3390/ijms23094642. DOI: https://doi.org/10.3390/ijms23094642
Steinhaus ME, Christ AB, Cross MB. Total knee arthroplasty for knee osteoarthritis: Support for a foregone conclusion? Musculoskelet J Hosp Spec Surg. 2017;13(2):207-210. doi: 10.1007/s11420-017-9558-4. DOI: https://doi.org/10.1007/s11420-017-9558-4
Da Silva RR, De Souza SR, Castro MM, Matos MA, Ariel De Lima D. Quality of life of patients submitted to total knee arthroplasty. J Health Biol Sci. 2024;12(1):1-9. doi: 10.12662/2317-3076jhbs.v12i1.4853.p1-9.2024. DOI: https://doi.org/10.12662/2317-3076jhbs.v12i1.4853.p1-9.2024
Luo D, Fan Z, Yin W. Chronic post-surgical pain after total knee arthroplasty: a narrative review. Perioper Med. 2024;13(1):108. doi: 10.1186/s13741-024-00466-9. DOI: https://doi.org/10.1186/s13741-024-00466-9
Arendt-Nielsen L, Skou ST, Nielsen TA, Petersen KK. Altered central sensitization and pain modulation in the CNS in chronic joint pain. Curr Osteoporos Rep. 2015;13(4):225-234. doi: 10.1007/s11914-015-0276-x. DOI: https://doi.org/10.1007/s11914-015-0276-x
Gandhi R, Santone D, Takahashi M, Dessouki O, Mahomed NN. Inflammatory predictors of ongoing pain 2 years following knee replacement surgery. The Knee. 2013;20(5):316-318. doi: 10.1016/j.knee.2012.10.015. DOI: https://doi.org/10.1016/j.knee.2012.10.015
Giordano R, Ghafouri B, Arendt-Nielsen L, Petersen KKS. Inflammatory biomarkers in patients with painful knee osteoarthritis: exploring the potential link to chronic postoperative pain after total knee arthroplasty—a secondary analysis. Pain. 2024;165(2):337-346. doi: 10.1097/j.pain.0000000000003042. DOI: https://doi.org/10.1097/j.pain.0000000000003042
Zhou D, Yang H, Zeng L, Yang W, Guo F, Cui W, et al. Calculated inflammatory markers derived from complete blood count results, along with routine laboratory and clinical data, predict treatment failure of acute peritonitis in chronic peritoneal dialysis patients. Ren Fail. 2023;45(1):2179856. doi: 10.1080/0886022X.2023.2179856. DOI: https://doi.org/10.1080/0886022X.2023.2179856
Marra A, Bondesan A, Caroli D, Sartorio A. Complete blood count (CBC)-derived inflammation indexes are useful in predicting metabolic syndrome in adults with severe obesity. J Clin Med. 2024;13(5):1353. doi: 10.3390/jcm13051353. DOI: https://doi.org/10.3390/jcm13051353
Tang Y, Zhai Y, Song W, Zhu T, Xu Z, Jiang L, et al. Association between complete blood count-derived inflammatory markers and the risk of frailty and mortality in middle-aged and older adults. Front Public Health. 2024;12:1427546. doi: 10.3389/fpubh.2024.1427546. DOI: https://doi.org/10.3389/fpubh.2024.1427546
Kriplani A, Pandit S, Chawla A, de la Rosette JJMCH, Laguna P, Jayadeva Reddy S, et al. Neutrophil-lymphocyte ratio (NLR), platelet-lymphocyte ratio (PLR) and lymphocyte-monocyte ratio (LMR) in predicting systemic inflammatory response syndrome (SIRS) and sepsis after percutaneous nephrolithotomy (PNL). Urolithiasis. 2022;50(3):341-348. doi: 10.1007/s00240-022-01319-0. DOI: https://doi.org/10.1007/s00240-022-01319-0
Taha SI, Samaan SF, Ibrahim RA, Moustafa NM, El-Sehsah EM, Youssef MK. Can complete blood count picture tell us more about the activity of rheumatological diseases? Clin Med Insights Arthritis Musculoskelet Disord. 2022;15:11795441221089182. doi: 10.1177/11795441221089182. DOI: https://doi.org/10.1177/11795441221089182
Moshfeghinia R, Najibi A, Moradi M, Assadian K, Ahmadi J. The association between hematological markers of inflammation and chronic cannabis use: a systematic review and meta-analysis of observational studies. Front Psychiatry. 2024;15:1438002. doi: 10.3389/fpsyt.2024.1438002. DOI: https://doi.org/10.3389/fpsyt.2024.1438002
Carrillo-Palau M, Vera-Santana B, Morant-Domínguez A, Hernández-Camba A, Ramos L, Alonso-Abreu I, et al. Hematological composite scores in patients with inflammatory bowel disease. J Clin Med. 2023;12(23):7248. doi: 10.3390/jcm12237248. DOI: https://doi.org/10.3390/jcm12237248
Patel DM, Patel DK, Patel MM, Patel LB, Shaikh RT, Shaikh NT, et al. Neutrophil-lymphocyte, lymphocyte-monocyte, and platelet-lymphocyte ratios: Non-invasive biomarkers for assessing inflammatory bowel disease activity. Recent Adv Inflamm Allergy Drug Discov. 2024;19. doi: 10.2174/0127722708330712241106074203. DOI: https://doi.org/10.2174/0127722708330712241106074203
Kosekli MA. Mean platelet volume and platelet to lymphocyte count ratio are associated with hepatitis B-related liver fibrosis. Eur J Gastroenterol Hepatol. 2022;34(3):324-327. doi: 10.1097/MEG.0000000000002219. DOI: https://doi.org/10.1097/MEG.0000000000002219
Munteanu AI, Jugănaru I, Nicoară DM, Mang N, Vasilescu R, Brad GF, et al. Evaluating the role of CBC-derived indices in children with Hashimoto’s thyroiditis. Diagnostics. 2024;14(24):2834. doi: 10.3390/diagnostics14242834. DOI: https://doi.org/10.3390/diagnostics14242834
Xu C, Guo H, Qu P, Fu J, Kuo FC, Chen JY. Preoperatively elevated serum inflammatory markers increase the risk of periprosthetic joint infection following total knee arthroplasty in patients with osteoarthritis. Ther Clin Risk Manag. 2018;14:1719-1724. doi: 10.2147/TCRM.S175854. DOI: https://doi.org/10.2147/TCRM.S175854
Ali KA, He L, Deng X, Pan J, Huang H, Li W. Assessing the predictive value of pre- and post-operative inflammatory markers in patients undergoing total knee arthroplasty. J Orthop Surg. 2024;19(1):614. doi: 10.1186/s13018-024-05104-0. DOI: https://doi.org/10.1186/s13018-024-05104-0
Nairn L, Sivaratnam S, Bali K, Wood TJ. Neutrophil to lymphocyte ratio as an indicator of periprosthetic joint infection: A retrospective cohort study. J Am Acad Orthop Surg. 2023. doi: 10.5435/JAAOS-D-23-00600. DOI: https://doi.org/10.5435/JAAOS-D-23-00600
Duran H, Alpdemir M, Çeken N, Alpdemir MF, Kula Atik T. Neutrophil/lymphocyte and platelet/lymphocyte ratios as a biomarker in postoperative wound infections. Turk J Biochem. 2022;47(6):756-762. doi: 10.1515/tjb-2021-0274. DOI: https://doi.org/10.1515/tjb-2021-0274
Jones IA, Wier J, Chen MS, Liu KC, Palmer R, Mayfield CK, et al. Complete Blood Count Ratios Predict Adverse Events After Total Joint Arthroplasty. J Am Acad Orthop Surg. 2024;32(24):e1315-e1323. doi: 10.5435/JAAOS-D-24-00184. DOI: https://doi.org/10.5435/JAAOS-D-24-00184
Dogru M, Yesiltepe Mutlu RG. The evaluation of neutrophil–lymphocyte ratio in children with asthma. Allergol Immunopathol (Madr). 2016;44(4):292-296. doi: 10.1016/j.aller.2015.09.005. DOI: https://doi.org/10.1016/j.aller.2015.09.005
Shoji F, Kozuma Y, Toyokawa G, Yamazaki K, Takeo S. Complete blood cell count-derived inflammatory biomarkers in early-stage non-small-cell lung cancer. Ann Thorac Cardiovasc Surg. 2020;26(5):248-255. doi: 10.5761/atcs.oa.19-00315. DOI: https://doi.org/10.5761/atcs.oa.19-00315
Aneez FA, Shariffdeen N, Haleem FA, Thangarajah BR, Rasaratnam K. Correlation between neutrophil to lymphocyte ratio and platelet to lymphocyte ratio with proteinuria in different stages of chronic kidney disease. Egypt J Intern Med. 2024;36(1):6. doi: 10.1186/s43162-023-00270-9. DOI: https://doi.org/10.1186/s43162-023-00270-9
Nanava N, Betaneli M, Giorgobiani G, Chikovani T, Janikashvili N. Complete blood count derived inflammatory biomarkers in patients with hematologic malignancies. Georgian Med News. 2020;(302):39-44.
Godoy G, Sumarriva G, Ochsner JL, Chimento G, Schmucker D, Dasa V, et al. Preoperative acute inflammatory markers as predictors for postoperative complications in primary total knee arthroplasty. Ochsner J. 2016;16(4):481-485.
Johnson AJ, Zywiel MG, Stroh A, Marker DR, Mont MA. Serological markers can lead to false negative diagnoses of periprosthetic infections following total knee arthroplasty. Int Orthop. 2011;35(11):1621-1626. doi: 10.1007/s00264-010-1175-5. DOI: https://doi.org/10.1007/s00264-010-1175-5
Costa L, Soares D, Aido R, Sousa R. The value of monitoring inflammatory markers after total joint arthroplasty. Hard Tissue. 2013;2(2). doi: 10.13172/2050-2303-2-2-410. DOI: https://doi.org/10.13172/2050-2303-2-2-410
Jaaban M, Zetoune AB, Hesenow S, Hessenow R. Neutrophil-lymphocyte ratio and platelet-lymphocyte ratio as novel risk markers for diabetic nephropathy in patients with type 2 diabetes. Heliyon. 2021;7(7):e07564. doi: 10.1016/j.heliyon.2021.e07564. DOI: https://doi.org/10.1016/j.heliyon.2021.e07564
Alirezaei A, Toudeshki KK, Taherian M, Pashapour H, Rahmani F, Norouzi N, et al. Comparison of complete blood count parameters in different severity of proteinuria among patients with type 2 diabetes mellitus. J Res Med Sci Off J Isfahan Univ Med Sci. 2024;29:66. doi: 10.4103/jrms.jrms_150_24.
Dainese P, Wyngaert KV, De Mits S, Wittoek R, Van Ginckel A, Calders P. Association between knee inflammation and knee pain in patients with knee osteoarthritis: a systematic review. Osteoarthritis Cartilage. 2022;30(4):516-534. doi: 10.1016/j.joca.2021.12.003. DOI: https://doi.org/10.1016/j.joca.2021.12.003
Rahimi-Levene N, Preisler Y, Koren-Michowitz M, Peer V, Zeidenstein R, Golik A, et al. Hematological biomarkers, mortality, transfusion and acute heart disease. Am J Med Sci. 2021;362(3):276-284. doi: 10.1016/j.amjms.2021.04.017. DOI: https://doi.org/10.1016/j.amjms.2021.04.017
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











