The Sensitivity of Immunohistochemical Expression of p53 as an Indicator of the Malignant Potential of Gastric Hyperplastic Polyps: A Retrospective Study
DOI:
https://doi.org/10.54133/ajms.v7i1.1235Keywords:
Dysplasia, Gastric polyps, Hyperplastic polyps, Immunohistochemistry, p53Abstract
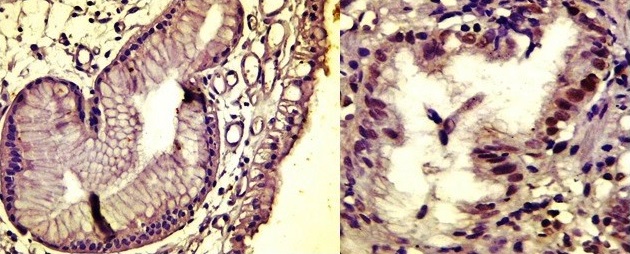
Background: Hyperplastic polyps account for 30–93% of gastric polyps. Recently, there have been studies about the development of dysplasia in this type of polyp. Every cell in the body contains the p53 gene, which has anti-cancer properties. Objective: The sensitivity of immunohistochemical expression of p53 is evaluated among gastric hyperplastic polyps with and without dysplasia and gastric adenomatous polyps to know its usefulness as a diagnostic marker. Methods: A retrospective cross-sectional study was done on fifty formalin-fixed paraffin-embedded blocks of gastric polyps (44 hyperplastic polyps without dysplasia, 3 hyperplastic polyps with dysplasia, and 3 adenomas). Cases were collected from the archives of the pathology department from June 2019 to July 2023. Additional sections of the block were immunostained with P53 protein. Results: Fifty paraffin blocks from patients with gastric polyps (17 males, 33 females) were included in the study. 44 of the cases are classified as hyperplastic polyps, 3 as hyperplastic polyps with dysplasia, and 3 as adenomatous polyps. Most gastric hyperplastic polyps showed staining in different scores. All gastric hyperplastic polyps with dysplasia showed nuclear staining, whereas two out of three gastric adenomatous polyps showed no staining. Conclusion: There was no significant association between p53 protein expression and the type of gastric polyps, the presence of intestinal metaplasia, or H. pylori. However, it has a significant correlation with the size of the polyps.
Downloads
References
Hu H, Zhang Q, Chen G, Pritchard DM, Zhang S. Risk factors and clinical correlates of neoplastic transformation in gastric hyperplastic polyps in Chinese patients. Sci Rep. 2020;10(1). doi: 10.1038/s41598-020-58900-z. DOI: https://doi.org/10.1038/s41598-020-58900-z
João M, Areia M, Alves S, Elvas L, Taveira F, Brito D, et al. Gastric hyperplastic polyps: A benign entity? Analysis of recurrence and neoplastic transformation in a cohort study. Portuguese J Gastroenterol. 2021;28(5):328–335. doi: 10.1159/000514714. DOI: https://doi.org/10.1159/000514714
Yantiss RK. Immunohistochemical and molecular features of gastric hyperplastic polyps. Adv Cytol Pathol. 2017;2(1). doi: 10.15406/acp.2017.02.00012. DOI: https://doi.org/10.15406/acp.2017.02.00012
Sionov RV, Haupt Y. The cellular response to p53: the decision between life and death. Oncogene. 1999;18(45):6145–6157. doi: 10.1038/sj.onc.1203130. DOI: https://doi.org/10.1038/sj.onc.1203130
Prives C, Hall PA. The p53 pathway. J Pathol. 1999;187(1):112–126. PMID: 10341712. DOI: https://doi.org/10.1002/(SICI)1096-9896(199901)187:1<112::AID-PATH250>3.3.CO;2-V
Vousden KH, Lu X. Live or let die: the cell's response to p53. Nat Rev Cancer. 2002;2(8):594-604. doi: 10.1038/nrc864. DOI: https://doi.org/10.1038/nrc864
Lacroix M, Toillon RA, Leclercq G. p53 and breast cancer, an update. Endocr Relat Cancer. 2006;13(2):293–325. doi: 10.1677/erc.1.01172. DOI: https://doi.org/10.1677/erc.1.01172
Kubbutat MHG, Jones SN, Vousden KH. Regulation of p53 stability by Mdm2. Nature. 1997;387(6630):299–303. doi: 10.1038/387299a0. DOI: https://doi.org/10.1038/387299a0
Markowski AR, Markowska A, Guzinska-Ustymowicz K. Pathophysiological and clinical aspects of gastric hyperplastic polyps. World J Gastroenterol. 2016;22(40):8883. doi: 10.3748/wjg.v22.i40.8883. DOI: https://doi.org/10.3748/wjg.v22.i40.8883
Zhang X, Wang M, Wang Y, Cheng X, Jiang Y, Xiao H. Clinicopathologic significance of Her-2 and P53 expressions in gastric cancer. Asian J Surg. 2023;46(1):526–531. doi: 10.1016/j.asjsur.2022.06.039. DOI: https://doi.org/10.1016/j.asjsur.2022.06.039
Kumar V, Abbas AK, Aster JC, (Eds.), Robbins Basic Pathology, (10th Ed.), Elsevier - Health Sciences Division, 2017.
Yamanaka K, Miyatani H, Yoshida Y, Ishii T, Asabe S, Takada O, et al. Malignant transformation of a gastric hyperplastic polyp in a context of Helicobacter pylori-negative autoimmune gastritis: a case report. BMC Gastroenterol. 2016;16(1). doi: 10.1186/s12876-016-0537-x. DOI: https://doi.org/10.1186/s12876-016-0537-x
Dascălu RI, Păduraru DN, Bolocan A, Ion D, Andronic O. The role of PET-CT in gastric cancer – A narrative review. Sudan J Med Sci. 2020;332–44332–44344. doi: 10.18502/sjms.v15i3.7749. DOI: https://doi.org/10.18502/sjms.v15i3.7749
Ahn JY, Son DH, Choi KD, Roh J, Lim H, Choi KS, et al. Neoplasms arising in large gastric hyperplastic polyps: endoscopic and pathologic features. Gastrointest Endosc. 2014;80(6):1005-1013. doi: 10.1016/j.gie.2014.04.020. DOI: https://doi.org/10.1016/j.gie.2014.04.020
Terada T. Malignant transformation of foveolar hyperplastic polyp of the stomach: a histopathological study. Med Oncol. 2010;28(4):941–944. doi: 10.1007/s12032-010-9556-6. DOI: https://doi.org/10.1007/s12032-010-9556-6
Yao T, Kajiwara M, Kuroiwa S, Iwashita A, Oya M, Kabashima A, et al. Malignant transformation of gastric hyperplastic polyps: Alteration of phenotypes, proliferative activity, and p53 expression. Hum Pathol. 2002;33(10):1016–1022. doi: 10.1053/hupa.2002.126874. DOI: https://doi.org/10.1053/hupa.2002.126874
Imura J, Hayashi S, Ichikawa K, Miwa S, Nakajima T, Nomoto K, et al. Malignant transformation of hyperplastic gastric polyps: An immunohistochemical and pathological study of the changes of neoplastic phenotype. Oncol Lett. 2014;7(5):1459–463. doi: 10.3892/ol.2014.1932. DOI: https://doi.org/10.3892/ol.2014.1932
Murakami K, Mitomi H, Yamashita K, Tanabe S, Saigenji K, Okayasu I. p53, but not c-Ki-ras, mutation and down-regulation of p21WAF1/CIP1and cyclin D1 are associated with malignant transformation in gastric hyperplastic polyps. Am J Clin Pathol. 2001;115(2):224–234. doi: 10.1309/VLF5-UCNH-XQM2-X410. DOI: https://doi.org/10.1309/VLF5-UCNH-XQM2-X410
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











