Electrocardiographic T-Wave Changes in Patients with Liver Cirrhosis: A Marker of Decompensation
DOI:
https://doi.org/10.54133/ajms.v9i2.2489Keywords:
Child-Pugh score, Cirrhotic cardiomyopathy, Diastolic dysfunction, Electrocardiographic changes, Liver cirrhosisAbstract
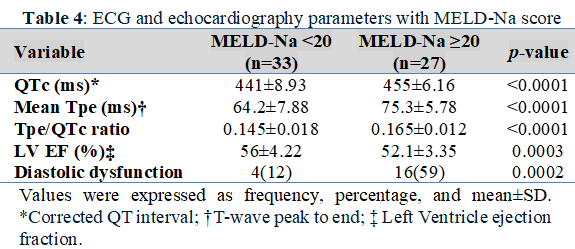
Background: Cirrhotic cardiomyopathy is an underrecognized complication that affects nearly half of patients with liver cirrhosis. Electrocardiographic T-wave changes and diastolic dysfunction may serve as an early sign of cardiac involvement. Objectives: To investigate the association between electrocardiographic and echocardiographic changes and/or the severity of liver cirrhosis, as well as estimated short-term mortality. Methods: This was an observational cross-sectional study conducted at Baghdad Teaching Hospital. Sixty patients with liver cirrhosis due to hepatitis B or hepatitis C viruses were enrolled in the study. Patients were grouped into three categories based on their Child-Pugh score and categorized into two groups based on the Model for End-stage Liver Disease (MELD-Na) score. We assess T-wave alterations in the ECG, together with systolic and diastolic dysfunction, to determine their correlation with the severity of liver cirrhosis and the likelihood of mortality within the subsequent months. Results: The average age of patients was 54.06 years. Seventeen patients had compensated liver cirrhosis, while 43 had decompensated disease (20 with category B and 23 with category C). There is a significant prolongation of QTc, prolongation of Tpe, an increase in the Tpe/QTc ratio, a reduction in left ventricle ejection fraction, and an increase in the percentage of diastolic dysfunction among patients with decompensated liver cirrhosis (Child-Pugh class B and C). Conclusions: Cirrhotic cardiomyopathy is related to the decompensation of liver cirrhosis. T-wave changes can be used as a marker of liver decompensation.
Downloads
References
Liu H, Ryu D, Hwang S, Lee SS. Therapies for cirrhotic cardiomyopathy: Current perspectives and future possibilities. Int J Mol Sci. 2024;25(11):5849. doi: 10.3390/ijms25115849. DOI: https://doi.org/10.3390/ijms25115849
Carvalho MVH, Kroll PC, Kroll RTM, Carvalho VN. Cirrhotic cardiomyopathy: the liver affects the heart. Braz J Med Biol Res. 2019;52(2):e7809. doi: 10.1590/1414-431X20187809. DOI: https://doi.org/10.1590/1414-431x20187809
Liu H, Nguyen HH, Yoon KT, Lee SS. Pathogenic mechanisms underlying cirrhotic cardiomyopathy. Front Netw Physiol. 2022;2:849253. doi: 10.3389/fnetp.2022.849253. DOI: https://doi.org/10.3389/fnetp.2022.849253
Izzy M, VanWagner LB, Lin G, Altieri M, Findlay JY, Oh JK, et al. Cirrhotic cardiomyopathy consortium. Redefining cirrhotic cardiomyopathy for the modern era. Hepatology. 2019;71:334–345. doi: 10.1002/hep.30875. Epub 2019 Oct 11. DOI: https://doi.org/10.1002/hep.30875
Zardi EM, Zardi DM, Chin D, Sonnino C, Dobrina A, Abbate A. Cirrhotic cardiomyopathy in the pre- and post-liver transplantation phase. J Cardiol. 2016;67(2):125–130. doi: 10.1016/j.jjcc.2015.04.016. DOI: https://doi.org/10.1016/j.jjcc.2015.04.016
Zardi EM, Abbate A, Zardi DM, Dobrina A, Margiotta D, Van Tassell BW, et al. Cirrhotic cardiomyopathy. J Am Coll Cardiol. 2010;56(7):539-549. doi: 10.1016/j.jacc.2009.12.075. DOI: https://doi.org/10.1016/j.jacc.2009.12.075
Izzy MJ, VanWagner LB. Current concepts of cirrhotic cardiomyopathy. Clin Liver Dis. 2021;25(2):471-481. doi: 10.1016/j.cld.2021.01.012. DOI: https://doi.org/10.1016/j.cld.2021.01.012
Bernardi M, Maggioli C, Dibra V, Zaccherini G. QT interval prolongation in liver cirrhosis: Innocent bystander or serious threat? Expert Rev Gastroenterol Hepatol. 2012;6:57-66. doi: 10.1586/egh.11.86. DOI: https://doi.org/10.1586/egh.11.86
Lee W, Vandenberk B, Raj SR, Lee SS. Prolonged QT interval in cirrhosis: twisting time? Gut Liver. 2022;16(6):849–860. doi: 10.5009/gnl210537. DOI: https://doi.org/10.5009/gnl210537
Mozos I. Arrhythmia risk in liver cirrhosis. World J Hepatol. 2015;7:662–672. doi: 10.4254/wjh.v7.i4.662. DOI: https://doi.org/10.4254/wjh.v7.i4.662
Bokarvadia R, Jain M, Kedarisetty C, Varghese J, Venkataraman J. Prevalence and clinical presentation of cirrhotic cardiomyopathy: A single centre experience from southern India. Indian J Gastroenterol. 2019;38(2):150-157. doi: 10.1007/s12664-019-00946-7. DOI: https://doi.org/10.1007/s12664-019-00946-7
Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019;70(1):151–171. doi: 10.1016/j.jhep.2018.09.014. DOI: https://doi.org/10.1016/j.jhep.2018.09.014
Reverter E, Tandon P, Augustin S, Turon F, Casu S, Bastiampillai R, et al. A MELD-based model to determine risk of mortality among patients with acute variceal bleeding. Gastroenterology. 2014;146(2):412-419. doi: 10.1053/j.gastro.2013.10.018. DOI: https://doi.org/10.1053/j.gastro.2013.10.018
Chen PC, Chen BH, Huang CH, Jeng WJ, Hsieh YC, Teng W, et al. Integrated model for end-stage liver disease may be superior to some other model for end-stage liver disease-based systems in addition to Child-Turcotte-Pugh and albumin-bilirubin scores in patients with hepatitis B virus-related liver cirrhosis and spontaneous bacterial peritonitis. Eur J Gastroenterol Hepatol. 2019;31(10):1256-1263. doi: 10.1097/MEG.0000000000001481. DOI: https://doi.org/10.1097/MEG.0000000000001481
Kim WR, Biggins SW, Kremers WK, Wiesner RH, Kamath PS, Benson JT, et al. Hyponatremia and mortality among patients on the liver-transplant waiting list. N Engl J Med. 2008;359(10):1018-1026. doi: 10.1056/NEJMoa0801209. DOI: https://doi.org/10.1056/NEJMoa0801209
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29(4):277–314. doi: 10.1016/j.echo.2016.01.011. DOI: https://doi.org/10.1016/j.echo.2016.01.011
Pinto C, Ninfole E, Gaggiano L, Benedetti A, Marzioni M, Maroni L. Aging and the biological response to liver injury. Semin Liver Dis. 2020;40(3):225-232. doi: 10.1055/s-0039-3402033. DOI: https://doi.org/10.1055/s-0039-3402033
Toma L, Stanciu AM, Zgura A, Bacalbasa N, Diaconu C, Iliescu L. Electrocardiographic Changes in Liver Cirrhosis-Clues for Cirrhotic Cardiomyopathy. Medicina (Kaunas). 2020 Feb 10;56(2):68. doi: 10.3390/medicina56020068. DOI: https://doi.org/10.3390/medicina56020068
Moaref A, Zamirian M, Yazdani M, Salehi O, Sayadi M, Aghasadeghi K. The correlation between echocardiographic findings and QT interval in cirrhotic patients. Int Cardiovasc Res J. 2014;8:39–43. PMID: 24936479.
Akboga MK, Yuksel M, Balci KG, Kaplan M, Cay S, Gokbulut V, et al. Tp-e interval, Tp-e/QTc ratio, and fragmented QRS are correlated with the severity of liver cirrhosis. Ann Noninvasive Electrocardiol. 2017;22(1):e12359. doi: 10.1111/anec.12359. DOI: https://doi.org/10.1111/anec.12359
Singh H, Panwar S, Arora R. Evaluation of electrocardiographic changes in patients with cirrhosis and their correlation with severity of disease. Int J Life Sci Biotechnol Pharma Res. 2023;12(3):477–482.
Testino G, Leone S, Pellicano R. Atrial fibrillation and alcoholic beverages. Minerva Med. 2019;110:471–472. doi: 10.23736/S0026-4806.19.05958-5. DOI: https://doi.org/10.23736/S0026-4806.19.05958-5
Tsiompanidis E, Siakavellas SI, Tentolouris A, Eleftheriadou I, Chorepsima S, Manolakis A, et al. Liver cirrhosis-effect on QT interval and cardiac autonomic nervous system activity. World J Gastrointest Pathophysiol. 2018;9:28–36. doi: 10.4291/wjgp.v9.i1.28. DOI: https://doi.org/10.4291/wjgp.v9.i1.28
Wong F. Cirrhotic cardiomyopathy. Hepatol Int. 2009;3:294–304. doi: 10.1007/s12072-008-9109-7. DOI: https://doi.org/10.1007/s12072-008-9109-7
Arteyeva NV, Goshka SL, Sedova KA, Bernikova OG, Azarov JE. What does the T(peak)-T(end) interval reflect? An experimental and model study. J Electrocardiol. 2013;46:296.e1–296. doi: 10.1016/j.jelectrocard.2013.02.001. DOI: https://doi.org/10.1016/j.jelectrocard.2013.02.001
Erikssen G, Liestøl K, Gullestad L, Haugaa KH, Bendz B, Amlie JP. The terminal part of the QT interval (T peak to T end): a predictor of mortality after acute myocardial infarction. Ann Noninvasive Electrocardiol. 2012;17(2):85-94. doi: 10.1111/j.1542-474X.2012.00493.x. DOI: https://doi.org/10.1111/j.1542-474X.2012.00493.x
Karaman K, Altunkaş F, Çetin M, Karayakali M, Arısoy A, Akar I, et al. New markers for ventricular repolarization in coronary slow flow: Tp-e interval, Tp-e/QT ratio, and Tp-e/QTc ratio. Ann Noninvasive Electrocardiol. 2015;20(4):338-344. doi: 10.1111/anec.12203. DOI: https://doi.org/10.1111/anec.12203
Barutcu S, Inanc I, Sabanoglu C, Polat E. Predictive value of Tp-e interval, Tp-e/QT, and Tp-e/QTc for disease severity in patients with liver cirrhosis. Eur Rev Med Pharmacol Sci. 2023;27(3):1110-1120. doi: 10.26355/eurrev_202302_31214.
Li X, Yu S, Li L, Han D, Dai S, Gao Y. Cirrhosis-related changes in left ventricular function and correlation with the model for end-stage liver disease score. Int J Clin Exp Med. 2014;7(12):5751-5757. PMID: 25664102.
Reddy YNV, Melenovsky V, Redfield MM, Nishimura RA, Borlaug BA. High-output heart failure: A 15-year experience. J Am Coll Cardiol. 2016;68(5):473–482. doi: 10.1016/j.jacc.2016.05.043. DOI: https://doi.org/10.1016/j.jacc.2016.05.043
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











