Histopathological Detection of Post-COVID-19 Fungal Co-infection in the Respiratory Tract
DOI:
https://doi.org/10.54133/ajms.v9i2.2343Keywords:
COVID-19, Fungal infection, Histopathology, Mucormycosis, Respiratory tract, Severity scoreAbstract
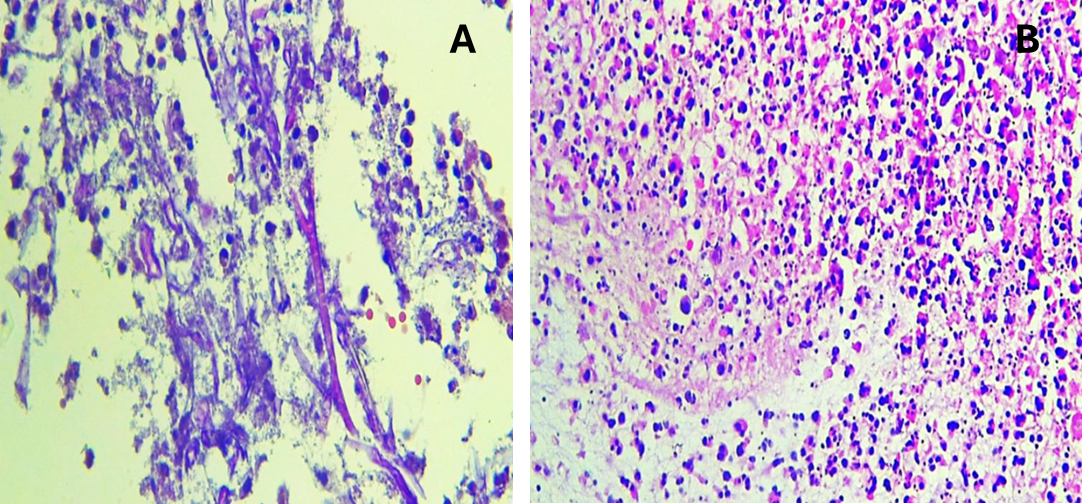
Background: Invasive fungal infections can complicate the clinical course of COVID-19, especially in severely ill patients who require admission to the intensive care unit. Objective: To evaluate the histopathological features and severity score of post-COVID-19 fungal co-infection in the respiratory tract in Ninevah Province and correlate the result with age, sex, and diabetes. Methods: Thirty patients who presented with post-COVID-19 fungal co-infection from August to May 2022 were involved in this retrospective case series study. Hematoxylin/eosin stain and periodic acid Schiff stain were used to stain the biopsies. Disease severity was assessed using a scoring system that incorporated grades from I to III across multiple histological variables. Results: Mucormycosis is the only fungal infection found in the samples received, with female predominance and an age of 54.20 years. Perinasal facial pain and swelling were the most common clinical presentations, and 76.7% were diabetics. Necrosis of ≥ 50% was observed in 63.3% of cases with a severe degree of neutrophilic infiltrate, and angioinvasion in more than 3 vessels in 10 high-power fields was identified in 60% of cases. Histologically, grade II was found in 50% of the cases. Conclusions: Post-COVID-19 patients have a significant risk of mucormycosis, in which diabetes and steroid administration were the most important predisposing factors in addition to systemic immune alteration in COVID-19-infected patients. Acute inflammation, tissue necrosis, fungal load, and angioinvasion were proposed.
Downloads
References
Casalini G, Giacomelli A, Ridolfo A, Gervasoni C, Antinori S. Invasive fungal infections complicating COVID-19: A narrative review. J Fungi (Basel). 2021;7(11):921. doi: 10.3390/jof7110921. DOI: https://doi.org/10.3390/jof7110921
Cevik M, Kuppalli K, Kindrachuk J, Peiris M. Virology, transmission, and pathogenesis of SARS-CoV-2. BMJ. 2020;371. doi: 10.1136/bmj.m3862. DOI: https://doi.org/10.1136/bmj.m3862
Ripa M, Galli L, Poli A, Oltolini C, Spagnuolo V, Mastrangelo A, et al. Secondary infections in patients hospitalized with COVID-19: Incidence and predictive factors. Clin Microbiol Infect. 2021;27(3):451–457. doi: 10.1016/j.cmi.2020.10.021. DOI: https://doi.org/10.1016/j.cmi.2020.10.021
Jensen HE. Histopathology in the diagnosis of invasive fungal diseases. Curr Fungal Infect Rep. 2021;15(1):23–31. doi: 10.1007/s12281-021-00412-y. DOI: https://doi.org/10.1007/s12281-021-00412-y
Jensen HE, Chandler FW. Histopathological diagnoses of mycoses. In: Merz WG, Hay RJ, (Eds), Topley & Wilson’s Medical Mycology, (10th ed.), London: Hodder Arnold; 2005.
Salehi M, Ahmadikia K, Badali H, Khodavaisy S. Opportunistic fungal infections in the epidemic area of COVID-19: a clinical and diagnostic perspective from Iran. Mycopathologia. 2020;185(4):607–611. doi: 10.1007/s11046-020-00472-7. DOI: https://doi.org/10.1007/s11046-020-00472-7
Jain K, Surana A, Choudhary TS, Vaidya S, Nandedkar S, Purohit M. Clinical and histological features as predictors of the severity of mucormycosis in post-COVID-19 patients: an experience from a rural tertiary setting in Central India. SAGE Open Med. 2022;10:205031212210747. doi: 10.1177/20503121221074744. DOI: https://doi.org/10.1177/20503121221074785
Jeong W, Keighley C, Wolfe R, Lee WL, Slavin MA, Kong DCM, et al. The epidemiology and clinical manifestations of mucormycosis: a systematic review and meta-analysis of case reports. Clin Microbiol Infect. 2019;25(1):26-34. doi: 10.1016/j.cmi.2018.07.011. DOI: https://doi.org/10.1016/j.cmi.2018.07.011
Pandiar D, Ramani P, Krishnan RP, Y D, Kumar NS, Gayathri R. Histopathological analysis of soft tissue changes in gingival biopsied specimen from patients with underlying coronavirus disease-associated mucormycosis. Med Oral Patol Oral Cir Bucal. 2022;27(3):e216–222. doi: 10.4317/medoral.24973. DOI: https://doi.org/10.4317/medoral.25050
Ahmadikia K, Hashemi SJ, Khodavaisy S, Getso MI, Alijani N, Badali H, et al. The double-edged sword of systemic corticosteroid therapy in viral pneumonia: a case report and comparative review of influenza-associated mucormycosis versus COVID-19-associated mucormycosis. Mycoses. 2021;64(8):798–808. doi: 10.1111/myc.13256. DOI: https://doi.org/10.1111/myc.13256
Global Nutrition Report. Country nutrition profiles – Iraq. Global Nutrition Report. 2022. Available from: https://globalnutritionreport.org/resources/nutrition-profiles/?country-search=Iraq.
Shahid Z, Kalayanamitra R, McClafferty B, Kepko D, Ramgobin D, Patel R, et al. COVID-19 and older adults: what we know. J Am Geriatr Soc. 2020;68(5):926–929. doi: 10.1111/jgs.16472. DOI: https://doi.org/10.1111/jgs.16472
Huang I, Pranata R, Lim MA, Oehadian A, Alisjahbana B. C-reactive protein, procalcitonin, D-dimer, and ferritin in severe coronavirus disease-2019: a meta-analysis. Ther Adv Respir Dis. 2020;14:1753466620937175. doi: 10.1177/1753466620937175. DOI: https://doi.org/10.1177/1753466620937175
Müller JA, Groß R, Conzelmann C, Krüger J, Merle U, Steinhart J, et al. SARS-CoV-2 infects and replicates in cells of the human endocrine and exocrine pancreas. Nat Metab. 2021;3(2):149–165. doi: 10.1038/s42255-021-00347-1. DOI: https://doi.org/10.1038/s42255-021-00347-1
Sree Lakshmi I, Kumari BS, Jyothi Ch, Devojee M, Padma Malini K, Sunethri P, et al. Histopathological study of mucormycosis in post-COVID-19 patients and factors affecting it in a tertiary care hospital. Int J Surg Pathol. 2022;30(5):498–505. doi: 10.1177/10668969221099661. DOI: https://doi.org/10.1177/10668969221099626
Morace G, Borghi E. Invasive mold infections: virulence and pathogenesis of Mucorales. Int J Microbiol. 2012;2012:349278. doi: 10.1155/2012/349278. DOI: https://doi.org/10.1155/2012/349278
Bayram N, Ozsaygılı C, Sav H, Tekin Y, Gundogan M, Pangal E, et al. Susceptibility of severe COVID-19 patients to rhino-orbital mucormycosis fungal infection in different clinical manifestations. Jpn J Ophthalmol. 2021;65(4):515–525. doi: 10.1007/s10384-021-00845-5. DOI: https://doi.org/10.1007/s10384-021-00845-5
Bhatt K, Agolli A, Patel MH, Garimella R, Devi M, Garcia E, et al. High mortality co-infections of COVID-19 patients: mucormycosis and other fungal infections. Discoveries (Craiova). 2021;9(1):e126. doi: 10.15190/d.2021.5. DOI: https://doi.org/10.15190/d.2021.5
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











