Polycystic Ovary Syndrome and Urinary Tract Stones: A Body Mass Index-Adjusted Analysis in Iraqi Women
DOI:
https://doi.org/10.54133/ajms.v8i1.1725Keywords:
BMI (Body Mass Index), Obesity, Overweight, Urinary stone, UnderweightAbstract
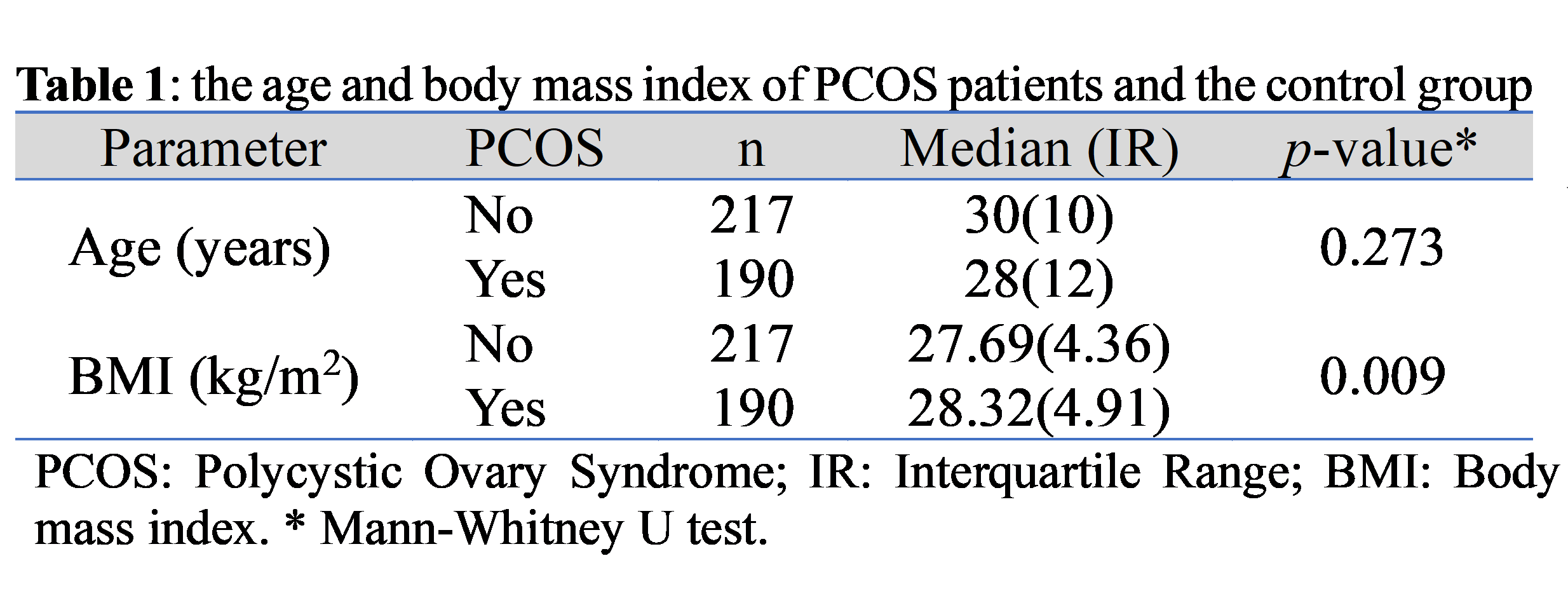
Background: Polycystic ovary syndrome (PCOS) has an unknown and complex etiology. It affects 5–10% of women in the reproductive age. Patients are known to have increased ovarian androgen production that is associated with decreased menses, hirsutism, and acne. Urinary tract stones (UTS) are a multifactorial disorder, with age and sex being known risk factors. Many PCOS patients are obese, and links between nephrolithiasis and obesity have been shown previously. Objectives: To identify the relation between PCOS and UTS considering the patients' body mass index (BMI). Methods: This is a cross-sectional study that enrolled 407 women aged 18-40 who attended the gynecology and obstetrics clinic at Al-Elwiya Maternity Teaching Hospital. The patients were assigned to the PCOS group or the control group. The data collected includes age, weight, height, body mass index (BMI), and the results of abdominal ultrasonography to detect UTS. Results: One hundred ninety women were in the PCOS group and 217 in the control group. The PCOS group had a higher BMI than the control group. Patients with UTS had a higher BMI than those without UTS. PCOS combined with a higher BMI showed an increased risk of having UTS. However, analysis of each of the variables taking the other into account showed no significant association. Conclusions: PCOS and BMI both raise the chances of having UTS; however, each one showed no significant association when adjusting for the other.
Downloads
References
Kaygusuz I, Karatas OF, Kafali H, Cimentepe E, Unal D. Is polycystic ovarian syndrome a risk factor for urolithiasis? Urolithiasis. 2013;41(4):361-362. doi: 10.1007/s00240-013-0564-9. DOI: https://doi.org/10.1007/s00240-013-0564-9
Adashi EY, Cibula D, Peterson M, Azziz R. The polycystic ovary syndrome: the first 150 years of study. F S Rep. 2022;4(1):2-18. doi: 10.1016/j.xfre.2022.12.002. DOI: https://doi.org/10.1016/j.xfre.2022.12.002
Singh S, Pal N, Shubham S, Sarma DK, Verma V, Marotta F, et al. Polycystic ovary syndrome: Etiology, current management, and future therapeutics. J Clin Med. 2023;12(4):1454. doi: 10.3390/jcm12041454. DOI: https://doi.org/10.3390/jcm12041454
Aziz ZN-E, Saleh BO, Thaker AZ. Free testosterone, dihydrotestosterone, and adiponectin in the evaluation of vitamin D supplementation for polycystic ovarian syndrome: A metformin comparative study. Al-Kindy Coll Med J. 2024;20(3):239-244. DOI: https://doi.org/10.47723/nb5he078
Abdull TN. Step-up protocol gonadotrophin versus laparoscopic ovarian drilling in clomiphene citrate resistant PCOS infertile women in two Iraqi hospitals. Al-Kindy Coll Med J. 2019;15(1):103-109. DOI: https://doi.org/10.47723/kcmj.v15i1.89
Bellver J, Rodríguez-Tabernero L, Robles A, Muñoz E, Martínez F, Landeras J, et al. Polycystic ovary syndrome throughout a woman's life. J Assist Reprod Genet. 2018;35(1):25-39. doi: 10.1007/s10815-017-1047-7. DOI: https://doi.org/10.1007/s10815-017-1047-7
Legro RS, Strauss JF. Molecular progress in infertility: polycystic ovary syndrome. Fertil Steril. 2002;78(3):569–576. doi: 10.1016/s0015-0282(02)03275-2. DOI: https://doi.org/10.1016/S0015-0282(02)03275-2
Rasquin LI, Anastasopoulou C, Mayrin JV. Polycystic ovarian disease. 2022 Nov 15. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024. PMID: 29083730.
Azziz R. Polycystic ovary syndrome. Obstet Gynecol. 2018;132(2):321-336. doi: 10.1097/AOG.0000000000002698. DOI: https://doi.org/10.1097/AOG.0000000000002698
Rostami Dovom M, Rahmati M, Amanollahi Soudmand S, Ziaeefar P, Azizi F, Ramezani Tehrani F. The hidden link between polycystic ovary syndrome and kidney stones: Finding from the Tehran Lipid and Glucose Study (TLGS). Diagnostics (Basel). 2023;13(17):2814. doi: 10.3390/diagnostics13172814. DOI: https://doi.org/10.3390/diagnostics13172814
Tahir NL, Hassan QA, Kamber HM. The prevalence of a clinically silent nephrolithiasis in Baghdad population: An initial ultrasound screening study from Iraq. Acta Medica Iranica. 2019:51-56. doi: 10.18502/acta.v57i1.1753. DOI: https://doi.org/10.18502/acta.v57i1.1753
Almannie RM, Al-Nasser KA, Al-Barraq KM, Alsheheli MM, Al-Hazmi HH, Binsaleh SA, et al. The effect of the body mass index on the types of urinary tract stones. Urol Ann. 2020;12(1):42-48. doi: 10.4103/UA.UA_161_18. DOI: https://doi.org/10.4103/UA.UA_161_18
Mosli HA, Mosli HH. Increased body mass index is associated with larger renal calculi. Urology. 2012;80:974-977. doi: 10.1016/j.urology.2012.07.027. DOI: https://doi.org/10.1016/j.urology.2012.07.027
Del Valle EE, Negri AL, Spivacow FR, Rosende G, Forrester M, Pinduli I. Metabolic diagnosis in stone formers in relation to body mass index. Urol Res. 2012;40(1):47-52. doi: 10.1007/s00240-011-0392-8. DOI: https://doi.org/10.1007/s00240-011-0392-8
Puttabyatappa M, Padmanabhan V. Ovarian and extra-ovarian mediators in the development of polycystic ovary syndrome. J Mol Endocrinol. 2018;61(4):R161-R184. doi: 10.1530/JME-18-0079. DOI: https://doi.org/10.1530/JME-18-0079
Rotterdam ESHRE/ASRM-Sponsored PCOS consensus workshop group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum Reprod. 2004;19(1):41-47. doi: 10.1093/humrep/deh098. DOI: https://doi.org/10.1093/humrep/deh098
Skolarikos A, Jung H, Neisius A, Petřík A, Somani B, Tailly T, et al. EAU Guidelines on Urolithiasis 2024. European Association of Urology 2024. Available from: https://uroweb.org/guidelines/urolithiasis
Cohen J. Statistical power analysis for the behavioral sciences. Routledge; 2013. doi: 10.4324/9780203771587. DOI: https://doi.org/10.4324/9780203771587
Fedrigon D, Alazem K, Sivalingam S, Monga M, Calle J. Nephrolithiasis and polycystic ovary syndrome: A case-control study evaluating testosterone and urinary stone metabolic panels. Adv Urol. 2019;2019:3679493. doi: 10.1155/2019/3679493. DOI: https://doi.org/10.1155/2019/3679493
Zhu X, Kaygusuz I, Eser A, Yildirim ME, Çimentepe E, Yüce E, et al. Is polycystic ovarian syndrome a risk factor for urinary stone disease? Clin Oncol. 2018;3:1443.
Jalilian N, Haghnazari L, Rasolinia S. Leptin and body mass index in polycystic ovary syndrome. Indian J Endocrinol Metab. 2016;20(3):324-328. doi: 10.4103/2230-8210.180005. DOI: https://doi.org/10.4103/2230-8210.180005
Fang Y, Liu L, Yang Y, Zhang B, Xie S. Causal association between BMI and polycystic ovarian syndrome: Bidirectional 2-sample mendelian randomization study. J Clin Endocrinol Metab. 2024;110(1):41-47. doi: 10.1210/clinem/dgae446. DOI: https://doi.org/10.1210/clinem/dgae446
Feng X, Wu W, Zhao F, Xu F, Han D, Guo X, et al. Relationship between body mass index and kidney stones based on dose-response analyses using restricted cubic splines applied to NHANES 2011-2016 data. J Ren Nutr. 2021;31(3):263-269. doi: 10.1053/j.jrn.2020.05.003. DOI: https://doi.org/10.1053/j.jrn.2020.05.003
Güler Y. Effects of body mass index on urinary lithogenic factors in urinary system stone patients. Folia Med (Plovdiv). 2024;66(1):80-87. doi: 10.3897/folmed.66.e114369. DOI: https://doi.org/10.3897/folmed.66.e114369
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











