Prevalence and Patterns of Ocular Comorbidities among Geriatric Population Residents in Rural Eastern India: A Cross-Sectional Study
DOI:
https://doi.org/10.54133/ajms.v7i1.1030Keywords:
Cataract, Diabetic retinopathy, Geriatric patients, Ocular morbidity, Refractive errorAbstract
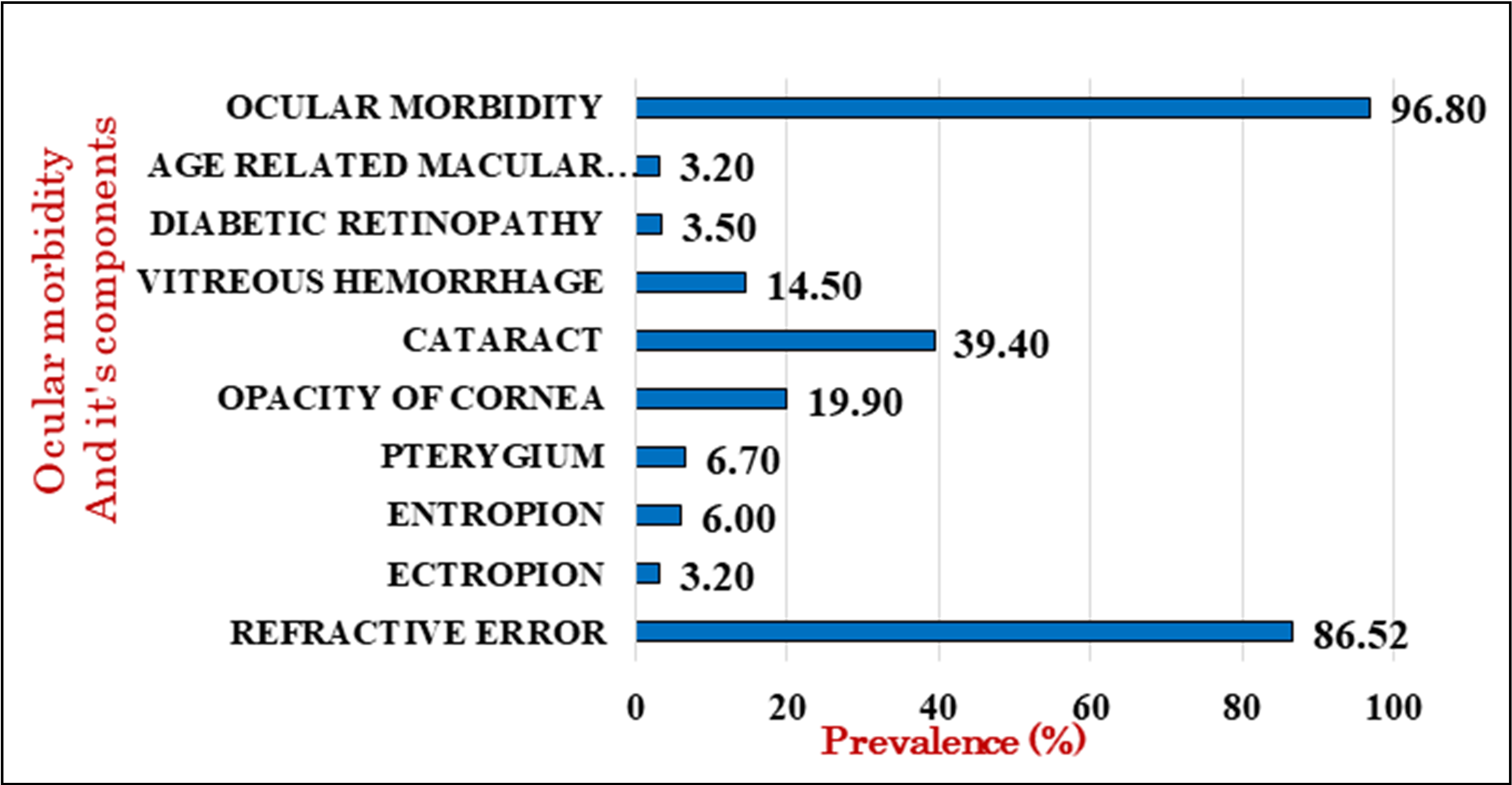
Background: With the increase in overall life expectancy, the number of people above 60 years old will increase globally from 1 billion in 2020 to 1.4 billion in 2050 and is expected to double by 2.1 billion by 2050 with an increase in age-related comorbidities. Age-related ocular co-morbidities are a major comorbidity. According to India's visual impairment and blindness data, cataracts and severe and moderate visual impairment are the most common cases. Objective: To assess the ocular comorbidities among the geriatric population. Methods: A community-based cross-sectional study was undertaken in the field practice area of the Rural Health Training Center (RHTC), Jamujhari, Khordha, affiliated with the Department of Community Medicine, IMS & SUM Hospital, Bhubaneswar. Stratified random sampling was done, and one stratum constituted three nearby adopted villages. Four strata were included to select the households, and the first household was selected randomly in each village. A socio-demographic profile and detailed clinical history were collected, and the required clinical examinations were conducted after obtaining consent. Results: The prevalence of ocular morbidity (OM) was found to be 96.8%. Refractive error (RE) has the highest prevalence (86.52%), including prescription-corrected glasses users, whereas age-related macular degeneration (ARMD) and ectropion (EC) have the lowest prevalence (3.2%). Conclusions: The study findings show a need for proactive management and earlier screening for better quality of life in the geriatric population.
Downloads
References
Ageing and health. [cited 2023 Mar 2]. Available from: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health
Bourne RRA, Steinmetz JD, Saylan M, Mersha AM, Weldemariam AH, Wondmeneh TG, et al. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: The Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;9(2):e144. PMID: 7820391.
Naipal S, Rampersad N. A review of visual impairment. Afr Vision Eye Health. 2018;77(1):4. doi.org/10.4102/aveh.v77i1.393. DOI: https://doi.org/10.4102/aveh.v77i1.393
Sarkar D, Sharma R, Singh P, Verma V, Karkhur S, Verma S, et al. Age-related cataract - Prevalence, epidemiological pattern and emerging risk factors in a cross-sectional study from Central India. Indian J Ophthalmol. 2023;71(5):1905-1912. doi: 10.4103/ijo.IJO_2020_22. DOI: https://doi.org/10.4103/ijo.IJO_2020_22
National Blindess and Visual Impairment Survey India 2015-19- A Summary Report - Google Search. [cited 2023 Mar 3]. Available from: https://www.google.com/search?client=firefox-b-d&q=National+Blindess+%26+Visual+Impairment+Survey+India+2015-19-+A+Summary+Report
Heald AH, Stedman M, Davies M, Livingston M, Alshames R, Lunt M, et al. Estimating life years lost to diabetes: outcomes from analysis of National Diabetes Audit and Office of National Statistics data. Cardiovasc Endocrinol Metab. 2020;9(4):183. PMID: 7673790. DOI: https://doi.org/10.1097/XCE.0000000000000210
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119. doi: 10.1016/j.diabres.2021.109119. DOI: https://doi.org/10.1016/j.diabres.2021.109119
Oberoi S, Kansra P. Economic menace of diabetes in India: a systematic review. Int J Diabetes Dev Ctries. 2020;40(4):464–4675. doi: 10.1007/s13410-020-00838-z. DOI: https://doi.org/10.1007/s13410-020-00838-z
Raman R, Vasconcelos JC, Rajalakshmi R, Prevost AT, Ramasamy K, Mohan V, et al. Prevalence of diabetic retinopathy in India stratified by known and undiagnosed diabetes, urban-rural locations, and socioeconomic indices: results from the SMART India population-based cross-sectional screening study. Lancet Glob Health. 2022;10(12):e1764–1773. doi: 10.1016/S2214-109X(22)00411-9. DOI: https://doi.org/10.1016/S2214-109X(22)00411-9
Teresi J, Morse AR, Holmes D, Yatzkan ES, Ramirez M, Rosenthal B, et al. Impact of a Vision Intervention on the Functional Status of Nursing Home Residents. J Visual Impair Blind. 2019;99(2):96–108. doi: 101177/0145482X0509900204. DOI: https://doi.org/10.1177/0145482X0509900204
Dev MK, Shrestha GS, Paudel N, Joshi ND, Thapa M, Shah DN. Visual status and ocular morbidity in older adults living in residential care. Graefes Arch Clin Exp Ophthalmol. 2012;250(9):1387-1393. doi: 10.1007/s00417-012-2056-y. DOI: https://doi.org/10.1007/s00417-012-2056-y
Mitchell P, Hinchcliffe P, Wang JJ, Rochtchina E, Foran S. Prevalence and associations with ectropion in an older population: the Blue Mountains Eye Study. Clin Exp Ophthalmol. 2001;29(3):108–110. doi: 10.1046/j.1442-9071.2001.00412.x. DOI: https://doi.org/10.1046/j.1442-9071.2001.00412.x
Sawada A, Tomidokoro A, Araie M, Iwase A, Yamamoto T. Refractive errors in an elderly Japanese population. The Tajimi study. Ophthalmology. 2008;115(2):363-370.e3. doi: 10.1016/j.ophtha.2007.03.075. DOI: https://doi.org/10.1016/j.ophtha.2007.03.075
Chen SJ, Tung TH, Liu JH, Lee AF, Lee FL, Hsu WM, et al. Prevalence and associated factors of refractive errors among type 2 diabetics in Kinmen, Taiwan. Ophthalmic Epidemiol. 2008;15(1):2–9. doi: 10.1080/09286580701585736. DOI: https://doi.org/10.1080/09286580701585736
Klein BEK, Klein R, Linton KLP. Prevalence of age-related lens opacities in a population: The Beaver Dam Eye Study. Ophthalmology. 1992;99(4):546–552. doi: 10.1016/s0161-6420(92)31934-7. DOI: https://doi.org/10.1016/S0161-6420(92)31934-7
Alabdulwahhab KM. Senile cataract in patients with diabetes with and without diabetic retinopathy: A community-based comparative study. J Epidemiol Glob Health. 2022;12(1):56–63. doi: 10.1007/s44197-021-00020-6. DOI: https://doi.org/10.1007/s44197-021-00020-6
Medical Science Monitor. Effect of turmeric and curcumin on oxidative stress and antioxidant enzymes in streptozotocin-induced diabetic rat. Article abstract #563761 [Internet]. [cited 2024 Feb 26]. Available from: https://medscimonit.com/abstract/index/idArt/563761
Klein BEK, Klein R, Moss SE. Prevalence of cataracts in a population-based study of persons with diabetes mellitus. Ophthalmology. 1985;92(9):1191–1196. doi: 10.1016/s0161-6420(85)33877-0. DOI: https://doi.org/10.1016/S0161-6420(85)33877-0
Yau JWY, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35(3):556–564. doi: 10.2337/dc11-1909. DOI: https://doi.org/10.2337/dc11-1909
Simó R, Stitt AW, Gardner TW. Neurodegeneration in diabetic retinopathy: does it really matter? Diabetologia. 2018;61(9):1902. doi: 10.1007/s00125-018-4692-1. DOI: https://doi.org/10.1007/s00125-018-4692-1
Antonetti DA, Barber AJ, Bronson SK, Freeman WM, Gardner TW, Jefferson LS, et al. Diabetic retinopathy seeing beyond glucose-induced microvascular disease. Diabetes. 2006;55(9):2401–2411. doi: 10.2337/db05-1635. DOI: https://doi.org/10.2337/db05-1635
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).