The Relationship Between Melasma and Thyroid Dysfunction—Analyzing Anti-thyroid Peroxidase Antibody Profiles: An Immuno-dermatological Perspective
DOI:
https://doi.org/10.54133/ajms.v9i2.2558Keywords:
Autoimmunity, Anti-TPO Antibodies, Melasma severity, mMASI, Thyroid autoantibodiesAbstract
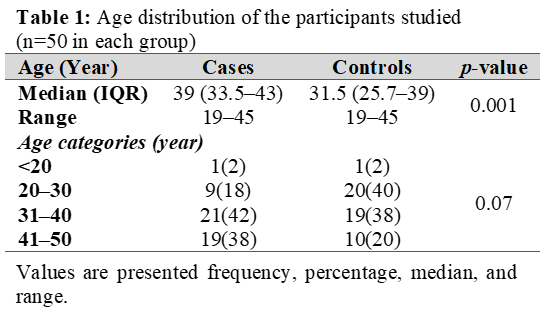
Background: Autoimmune mechanisms have been increasingly implicated in pigmentary disorders such as melasma. Thyroid autoimmunity, reflected by anti-thyroid peroxidase (anti-TPO) antibodies, can influence melanogenesis and disease severity. Objective: To evaluate the correlation between melasma severity and anti-TPO antibody levels. Methods: Fifty people with melasma took part in this case-control study and had their mMASI score and serum anti-TPO antibody levels evaluated. Age-matched controls (n=50) were included for comparison. Results: The mean anti-TPO level is significantly higher in melasma cases compared to controls (24.9±7.3 vs. 19.5±7.9; p=0.001). Within the melasma group, anti-TPO levels show a strong positive correlation with mMASI (r= 0.4, p=0.001), and age (r= 0.3, p=0.001). Melasma severity was higher in older age groups (p= 0.001). Conclusions: Anti-TPO antibodies are elevated in melasma and correlate with disease severity, supporting a potential autoimmune contribution to melasma pathogenesis.
Downloads
References
comprehensive review. Dermatol Ther (Heidelb). 2017;7(3):305-318. doi: 10.1007/s13555-017-0194-1.
Çakmak SK, Özcan N, Kılıç A, Koparal S, Artüz F, Çakmak A, et al. Etiopathogenetic factors, thyroid functions and thyroid autoimmunity in melasma patients. Postepy Dermatol Alergol. 2015;32(4):327-330. doi: 10.5114/pdia.2015.54742.
Raimondi S, Suppa M, Gandini S. Melanoma epidemiology and sun exposure. Acta Derm Venereol. 2020;100(adv00136):1-10. doi: 10.2340/00015555-3491.
Ali L, Al Niaimi F. Pathogenesis of melasma explained. Int J Dermatol. 2025;64(10):1201-1212. doi: 10.1111/ijd.17718.
Jang YH, Lee JY, Kang HY, Lee ES, Kim YC. Oestrogen and progesterone receptor expression in melasma: An immunohistochemical analysis. J Eur Acad Dermatol Venereol. 2010;24(11):1312-1316. doi: 10.1111/j.1468-3083.2010.03638.x.
Aishwarya K, Bhagwat PV, John N. Current concepts in melasma: A review article. J Skin Sex Transm Dis. 2020;2(1):13-19. doi: 10.25259/JSSTD_34_2019.
Fröhlich E, Wahl R. Thyroid autoimmunity: role of anti-thyroid antibodies in thyroid and extra-thyroidal diseases. Front Immunol. 2017;8(521):1-10. doi: 10.3389/fimmu.2017.00521.
Rostami Mogaddam M, Iranparvar Alamdari M, Maleki N, Safavi Ardabili N, Abedkouhi S. Evaluation of autoimmune thyroid disease in melasma. J Cosmet Dermatol. 2015;14(2):167–171. doi: 10.1111/jocd.12138.
Basit H, Godse KV, Al Aboud AM. Melasma. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2025. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459271/
Handel AC, Miot LDB, Miot HA. Melasma: a clinical and epidemiological review. An Bras Dermatol. 2014;89(5):771–782. doi: 10.1590/abd1806-4841.20143063.
Espósito ACC, Cassiano DP, da Silva CN, Lima PB, Dias JAF, Hassun K, et al. Update on Melasma – Part I: Pathogenesis. Dermatol Ther (Heidelb). 2022;12(9):1967–1988. doi: 10.1007/s13555-022-00779-x.
Mpofana N, Paulse M, Gqaleni N, Makgobole MU, Pillay P, Hussein A, et al. The effect of melasma on the quality of life in people with darker skin types living in Durban, South Africa. Int J Environ Res Public Health. 2023;20(2):7068. doi: 10.3390/ijerph20227068.
Lutfi RJ, Fridmanis M, Misiunas AL, Pafume O, Gonzalez EA, Villemur JA, et al. Association of melasma with thyroid autoimmunity and other thyroidal abnormalities and their relationship to the origin of the melasma. J Clin Endocrinol Metab. 1985;61(1):28–31. doi: 10.1210/jcem-61-1-28.
Saunders LM, Mishra AK, Aman AJ, Lewis VM, Toomey MB, Packer JS, et al. Thyroid hormone regulates distinct paths to maturation in pigment cell lineages. Elife. 2019;8:e45181. doi: 10.7554/eLife.45181.
Kheradmand M, Afshari M, Damiani G, Abediankenari S, Moosazadeh M. Melasma and thyroid disorders: a systematic review and meta-analysis. Int J Dermatol. 2019;58(10):1231–1238. doi: 10.1111/ijd.14497.
.Al-Shamma YMH, Al-Wakeel HA, Al-Awadi IJM. The prevalence of thyroid disorders in patients with melasma. Al-Qadisiyah Med J. 2017;12(21):107–111. doi: 10.28922/qmj.2016.12.21.107-111.
Ameneh Y, Banafsheh H. Association of melasma with thyroid autoimmunity: a case–control study. Iran J Dermatol. 2010;13(2):51–53..
Achar Achar A, Rathi SK. Melasma: a clinico-epidemiological study of 312 cases. Indian J Dermatol. 2011;56(4):380–382. doi: 10.4103/0019-5154.84722.
Liu W, Chen Q, Xia Y. New mechanistic insights of melasma. Clin Cosmet Investig Dermatol. 2023;16(1):429–442. doi: 10.2147/CCID.S396272.
Prabha N, Mahajan VK, Mehta KS, Chauhan PS, Gupta M. Cosmetic contact sensitivity in patients with melasma: results of a pilot study. Dermatol Res Pract. 2014;2014:316219. doi: 10.1155/2014/316219.
Sardesai VR, Kolte JN, Srinivas BN. A clinical study of melasma and comparison of the therapeutic effect of certain currently available topical modalities for its treatment. Indian J Dermatol. 2013;58(3):239–242. doi: 10.4103/0019-5154.110842.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











