Health Seeking Behavior and Medication Adherence of Hypertensive Patients in Erbil City: A Cross-Sectional Study
DOI:
https://doi.org/10.54133/ajms.v9i1.2313Keywords:
Hypertension, Hypertensive patients, Health-seeking behavior, Medication adherenceAbstract
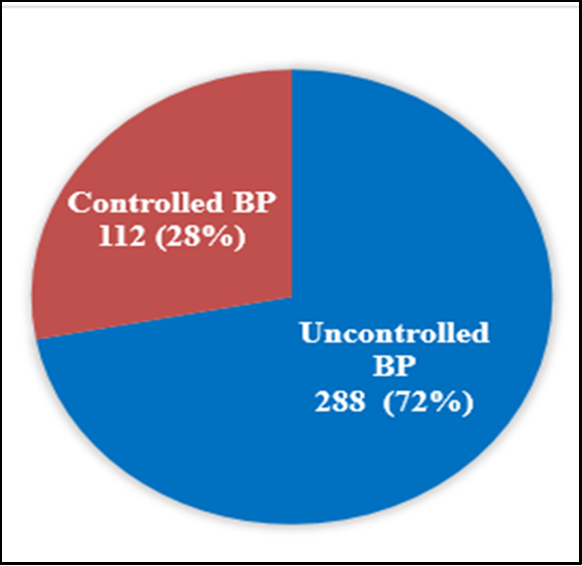
Background: Hypertension is a serious public health problem globally. Many patients don’t adhere to the treatment plan, even though treatment is freely available. Objective: To assess health-seeking behavior and drug adherence among a group of hypertensive patients. Methods: 400 hypertensive patients participated in a cross-sectional study done in Erbil, Kurdistan region, Iraq. Data were gathered through face-to-face interviews using a structured questionnaire that encompassed demographic variables, health-seeking behavior, medication adherence, barriers, and social support. Results: Most of the patients were males (82%), urban residents (74.25%), and aged ≥70 years. Obesity (42.75%) and overweight (41%) were common. 44.5% had high socioeconomic status. Overall, 74.5% adhered to medication regimens. No significant associations were found between adherence and demographic or socioeconomic factors. 66.3% used combination medication and lifestyle changes. Uncontrolled BP was prevalent (72%), and 25.5% were non-adherent, though non-adherence was not significantly associated with uncontrolled BP. Social support was common but did not significantly impact adherence. Among respondents, 125(31.3%) reported facing barriers to BP control. The most reported barriers were personal negligence (63.2%) and medication costs (43.2%). There is no exclusive barrier that has a significant association separately. Conclusions: Despite treatment adherence, most participants had uncontrolled BP. Social support and demographic characteristics had no impact on adherence. Poor control was mainly due to the irregular pattern of blood pressure monitoring, the preference for home-based checks, expense, and personal neglect.
Downloads
References
Sambah F, McBain-Rigg K, Seidu AA, Emeto. Interpersonal factors influencing hypertension control. : A cross-sectional study among hypertensive patients in the Ashanti Region, Ghana. Health Sci Rep. 2025;8(3):e70519. doi: 10.1002/hsr2.70519. DOI: https://doi.org/10.1002/hsr2.70519
Gay HC, Rao SG, Vaccarino V, Ali MK. Effects of different dietary interventions on blood pressure: systematic review and meta-analysis of randomized controlled trials. Hypertension. 2016 Apr;67(4):733–739. doi: 10.1161/HYPERTENSIONAHA.115.06853. DOI: https://doi.org/10.1161/HYPERTENSIONAHA.115.06853
Boateng EB, Ampofo AG. A glimpse into the future: modelling global prevalence of hypertension. BMC Public Health. 2023;23:1906. doi: 10.1186/s12889-023-16662-z. DOI: https://doi.org/10.1186/s12889-023-16662-z
Zaky NH. The relationship between health locus of control, knowledge, and adherence to antihypertensive regimen among women with preeclampsia. Am J Nurs Res. 2016;4(2):41–50. doi: 10.12691/ajnr-4-2-3.
Okati-Aliabad H, Ansari-Moghaddam A, Kargar S, Mohammadi M. Prevalence of hypertension and pre-hypertension in the Middle East region: a systematic review and meta-analysis. J Hum Hypertens. 2022;36:794–804. doi: 10.1038/s41371-021-00647-9. DOI: https://doi.org/10.1038/s41371-021-00647-9
Saka M, Shabu S, Shabila N. Prevalence of hypertension and associated risk factors in older adults in Kurdistan, Iraq. East Mediterr Health J. 2020;26(3):268–275. doi: 10.26719/emhj.19.029. DOI: https://doi.org/10.26719/emhj.19.029
Amen SO, Rasool BQ, Muhammad HM. Hypertension in Iraq. Med J Babylon. 2021;18(3):275. doi: 10.4103/MJBL.MJBL_24_21. DOI: https://doi.org/10.4103/MJBL.MJBL_24_21
Balouchi A, Rafsanjani MHAP, Al-Mutawaa K, Naderifar M, Rafiemanesh H, Ebadi A, et al. Hypertension and pre-hypertension in Middle East and North Africa (MENA): A meta-analysis of prevalence, awareness, treatment, and control. Curr Probl Cardiol. 2022;47(7):101069. doi: 10.1016/j.cpcardiol.2021.101069. DOI: https://doi.org/10.1016/j.cpcardiol.2021.101069
Sarki AM, Nduka CU, Stranges S, Kandala NB, Uthman OA. Prevalence of hypertension in low- and middle-income countries: a systematic review and meta-analysis. Medicine (Baltimore). 2015;94(50):e1959. doi: 10.1097/MD.0000000000001959. DOI: https://doi.org/10.1097/MD.0000000000001959
Matsumura K, Arima H, Tominaga M, Ohtsubo T, Sasaguri T, Fujii K, et al. Impact of antihypertensive medication adherence on blood pressure control in hypertension: the COMFORT study. QJM. 2013;106(10):909–914. doi: 10.1093/qjmed/hct121. DOI: https://doi.org/10.1093/qjmed/hct121
Brannon L, Feist J, Updegraff JA. Seeking and receiving health care. In: Brannon L, Feist J, Updegraff JA, (Eds.), Health psychology: An introduction to behavior and health, (9th ed.), Boston (MA): Cengage Learning; 2018. p. 41–60.
Pirouz M, Yavari M, Shojaeizadeh D, Vahedian-Shahroodi M, Fallahzadeh H. Awareness: the golden key to understanding healthcare seeking behavior among elderly hypertensive patients in Taft, Iran. Elderly Health J. 2024;10(1):62–69. doi: 10.18502/ehj.v10i1.15967. DOI: https://doi.org/10.18502/ehj.v10i1.15967
Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. doi: 10.1097/00005650-198601000-00007. DOI: https://doi.org/10.1097/00005650-198601000-00007
Al Meslamani AZ. Policy solutions for medication non-adherence: what can governments do? Expert Rev Pharmacoecon Outcomes Res. 2024;24(7):777–781. doi:10.1080/14737167.2024.2321242. DOI: https://doi.org/10.1080/14737167.2024.2321242
Jansen EM, van de Hei SJ, Dierick BJH, Kerstjens HAM, Kocks JWH, van Boven JFM, et al. Global burden of medication non-adherence in chronic obstructive pulmonary disease (COPD) and asthma: a narrative review of the clinical and economic case for smart inhalers. J Thorac Dis. 2021;13(6):3846–3864. doi: 10.21037/jtd-20-2360. DOI: https://doi.org/10.21037/jtd-20-2360
Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47(6):555–567. doi: 10.1016/S0022-3999(99)00057-4. DOI: https://doi.org/10.1016/S0022-3999(99)00057-4
TechRadar. Best smart scales 2025: Weigh up the best options for you [Internet]. 2021 [cited 2025 Jun 30]. Available from: https://www.techradar.com/best/best-smart-scales
Kario K, Okura A, Hoshide S, Mogi M. The WHO Global Report 2023 on hypertension: warning of the emerging global burden and its treatment strategy. Hypertens Res. 2024;47(5):1099–1102. doi: 10.1038/s41440-024-01510-6. DOI: https://doi.org/10.1038/s41440-024-01622-w
Wang TD, Ohkubo T, Bunyi ML, Chadachan VM, Chia YC, Kario K, et al. Current realities of home blood pressure monitoring from physicians’ perspectives: results from Asia HBPM survey 2020. Hypertens Res. 2023;46(7):1638–1649. doi: 10.1038/s41440-023-01318-1. DOI: https://doi.org/10.1038/s41440-023-01259-1
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension. 2020;75(6):1334–1357 doi:10.1161/HYPERTENSIONAHA.120.15026. DOI: https://doi.org/10.1161/HYPERTENSIONAHA.120.15026
Rhee MY, Munakata M, Nah DY, Kim JS, Kim HY. Home blood pressure measurement for hypertension management in the real world: Do not just measure, but share with your physician. Front Cardiovasc Med. 2023;10:1103216. doi: 10.3389/fcvm.2023.1103216. DOI: https://doi.org/10.3389/fcvm.2023.1103216
Sutton J, Gu L, Diercks DB. Impact of social determinants of health, health literacy, self-perceived risk, and trust in the emergency physician on compliance with follow-up. West J Emerg Med. 2021;22(3):667–671. doi: 10.5811/westjem.2020.12.48981. DOI: https://doi.org/10.5811/westjem.2020.12.48981
Studer CM, Linder M, Pazzagli L. A global systematic overview of socioeconomic factors associated with antidiabetic medication adherence in individuals with type 2 diabetes. J Health Popul Nutr. 2023;42:122. doi: 10.1186/s41043-023-00459-2. DOI: https://doi.org/10.1186/s41043-023-00459-2
Forouzan Z, Gholamrezaie A, Nasimi H, Faramarzi M, Bagheri-Ghalehsalimi A, Nourian SM, et al. Factors associated with adherence to treatment in Iranian patients with inflammatory bowel disease. J Res Med Sci. 2021;26:92. doi: 10.4103/jrms.JRMS_866_16. DOI: https://doi.org/10.4103/jrms.JRMS_866_16
Burch P, Walter A, Stewart S, Robertson L, Hall Dykgraaf S, McDonald J. Patient reported measures of continuity of care and health outcomes: a systematic review. BMC Prim Care. 2024;25:309. doi: 10.1186/s12875-024-02545-8. DOI: https://doi.org/10.1186/s12875-024-02545-8
Houchens N, Engle JM, Palanjian R, Nordstrom B, Kanzaria HK, Chui K, et al. Effect of clinician posture on patient perceptions of communication in the inpatient setting: a systematic review. J Gen Intern Med. 2024;39:3290–3298. doi: 10.1007/s11606-024-08906-4. DOI: https://doi.org/10.1007/s11606-024-08906-4
Tam HL, Wong EML, Cheung K. Effectiveness of educational interventions on adherence to lifestyle modifications among hypertensive patients: an integrative review. Int J Environ Res Public Health. 2020;17(7):2513. doi: 10.3390/ijerph17072513. DOI: https://doi.org/10.3390/ijerph17072513
SEC Working Group for the 2024 ESC guidelines for the management of elevated blood pressure and hypertension and SEC Guidelines Committee. Comments on the 2024 ESC guidelines for the management of elevated blood pressure and hypertension. Rev Esp Cardiol. 2025;78(4):296–300. doi: 10.1016/j.rec.2024.11.018. DOI: https://doi.org/10.1016/j.rec.2024.11.018
Zhou X, Zhang X, Gu N, Cai W, Feng J. Barriers and facilitators of medication adherence in hypertension patients: a meta-integration of qualitative research. J Patient Exp. 2024;11. doi: 10.1177/23743735241241176. DOI: https://doi.org/10.1177/23743735241241176
Sanuade OA, Ale BM, Baldridge AS, Orji IA, Shedul GL, Ojo TM, et al. Fixed-dose combination therapy-based protocol compared with free pill combination protocol: results of a cluster randomized trial. J Clin Hypertens (Greenwich). 2023;25(1):88–98. doi: 10.1111/jch.14632. DOI: https://doi.org/10.1111/jch.14632
Mansoor AR, Abed A, Alqudah A, Alsayed AR. Assessment of medical care strategies for primary hypertension in Iraqi adults: a hospital-based problem-oriented plan. Patient Prefer Adherence. 2025;19:1317–1335. doi: 10.2147/PPA.S510908. DOI: https://doi.org/10.2147/PPA.S510908
Ahmadi Z, Shahnazi H, Hassanzadeh A. Evaluation of medication adherence and its relevant factors among hypertensive patients: a cross-sectional study in Shahrekord health-care system. J Educ Health Promot. 2022;11:223. doi: 10.4103/jehp.jehp_1332_21. DOI: https://doi.org/10.4103/jehp.jehp_1332_21
Edward A, Campbell B, Manase F, Lufungulo D, Lwambano A, Mayumana I, et al. Patient and healthcare provider perspectives on adherence with antihypertensive medications: an exploratory qualitative study in Tanzania. BMC Health Serv Res. 2021;21:834. doi: 10.1186/s12913-021-06858-7. DOI: https://doi.org/10.1186/s12913-021-06858-7
Burnier M, Egan BM. Adherence in hypertension. Circ Res. 2019;124(7):1124–1140. doi: 10.1161/CIRCRESAHA.118.313220. DOI: https://doi.org/10.1161/CIRCRESAHA.118.313220
Aminde LN, Agbor VN, Fongwen NT, Ngwasiri CA, Nkoke C, Nji MA, et al. High burden and trend in nonadherence to blood pressure-lowering medications: meta-analysis of data from over 34 000 adults with hypertension in sub-Saharan Africa. J Am Heart Assoc. 2025;14(9):e037555. doi: 10.1161/JAHA.124.037555. DOI: https://doi.org/10.1161/JAHA.124.037555
Charchar FJ, Prestes PR, Mills C, Ching SM, Neupane D, Marques FZ, et al. Lifestyle management of hypertension: International Society of Hypertension position paper endorsed by the World Hypertension League and European Society of Hypertension. J Hypertens. 2024;42(1):23–49. doi: 10.1097/HJH.0000000000003563. DOI: https://doi.org/10.1097/HJH.0000000000003563
Jhaj R, Gour PR, Kumari S, Sharma S. Association between medication adherence and blood pressure control in urban hypertensive patients in central India. Int J Noncommunicable Dis. 2018;3(1):9–14. doi: 10.4103/jncd.jncd_29_16. DOI: https://doi.org/10.4103/jncd.jncd_29_16
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











