New Trials in Iraqi Hospitals to Manage Pain After Excisional Hemorrhoidectomy
DOI:
https://doi.org/10.54133/ajms.v9i1.2156Keywords:
Analgesia, Excisional hemorrhoidectomy, Postoperative pain controlAbstract
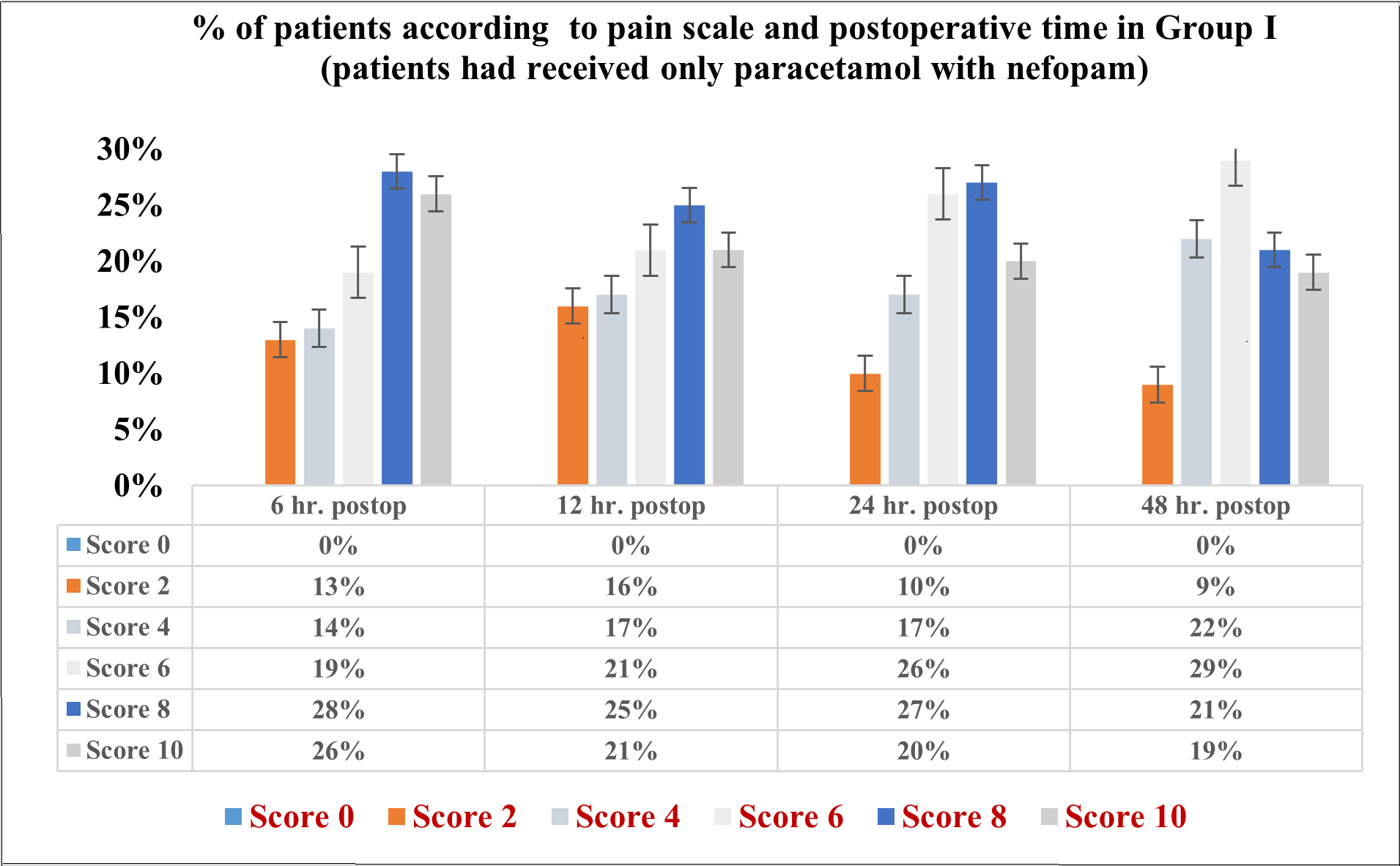
Background: Excisional hemorrhoidectomy is well-documented to be the best operation for high-grade hemorrhoids as well as complicated hemorrhoids. Yet, postoperative pain is still an exciting problem. Objective: To identify the best synergistic pharmacological mode used for reducing post-excisional hemorrhoidectomy pain. Methods: In a randomized study, 400 patients attending Al-Khadraa' Private Hospital, Baghdad, during the period from June 2022 to January 2024 were allocated into 4 groups (100 in each) according to type of anesthesia and analgesia at intraoperative as well as postoperative management. All underwent excisional hemorrhoidectomy according to the surgeon’s decision. Group I received paracetamol with nefopam; Group II received paracetamol, nefopam, ketamine, and fentanyl; Group III received paracetamol, nefopam, ketamine, fentanyl, and tramadol; and Group IV received paracetamol, nefopam, fentanyl, tramadol, and pethidine. Results: Group I reported the highest pain scores across all time points. Group II and Group III showed moderate improvement in pain control. Group IV demonstrated the lowest pain scores throughout, with a higher percentage of patients reporting minimal or no pain. Data analysis revealed a significant difference in pain scores between groups, and Group IV had significantly lower pain levels compared to the other groups. Conclusions: Though there are dissimilarities in the drug methodology in different studies, some Iraqi strategies to reduce post-hemorrhoidectomy pain are presented in this work; however, the combination of paracetamol, nefopam, fentanyl, tramadol, and pethidine had the best effect.
Downloads
References
Cristea C, Lewis CR, (Eds.), Hemorrhoidectomy. StatPearls. Treasure Island (FL): StatPearls Publishing; 2024 Jan. Updated 2024 Feb 24. PMID: 31751054.
Gallo G, Goglia M, Trompetto M. Postoperative pain after haemorrhoidal disease treatment: a still unsolved problem. Tech Coloproctol. 2024;28(6). doi: 10.1007/s10151-023-02889-w. DOI: https://doi.org/10.1007/s10151-023-02889-w
Eberspacher C, Mascagni D, Pontone S, Arcieri FL, Arcieri S. Topical metronidazole after haemorrhoidectomy to reduce postoperative pain: a systematic review. Updates Surg. 2024;76(4):1161-1167. doi: 10.1007/s13304-024-01930-3. DOI: https://doi.org/10.1007/s13304-024-01930-3
Lohsiriwat V. Approach to hemorrhoids. Curr Gastroenterol Rep. 2013;15:332. doi: 10.1007/s11894-013-0332-6. DOI: https://doi.org/10.1007/s11894-013-0332-6
Picciariello A, Tsarkov PV, Papagni V, Efetov S, Markaryan DR, Tulina I, et al. Classifications and clinical assessment of haemorrhoids: The proctologist’s corner. Rev Recent Clin Trials. 2021;16:10–16. doi: 10.2174/1574887115666200312163940. DOI: https://doi.org/10.2174/1574887115666200312163940
Lohsiriwat V. Treatment of hemorrhoids: A coloproctologist’s view. World J Gastroenterol. 2015;21:9245–9252. doi: 10.3748/wjg.v21.i31.9245. DOI: https://doi.org/10.3748/wjg.v21.i31.9245
Bhatti MI, Sajid MS, Baig MK. Milligan–Morgan (open) versus Ferguson haemorrhoidectomy (closed): A systematic review and meta-analysis of published randomized, controlled trials. World J Surg. 2016;40:1509–1519. doi: 10.1007/s00268-016-3419-z. DOI: https://doi.org/10.1007/s00268-016-3419-z
Langenbach MR, Florescu RV, Köhler A, Barkus J, Ritz JP, Quemalli E, et al. Tamponade dressing versus no dressing after haemorrhoidectomy: multicentre, randomized clinical trial. BJS Open. 2022;6(3):zrac070. doi: 10.1093/bjsopen/zrac070. DOI: https://doi.org/10.1093/bjsopen/zrac070
Lohsiriwat V. Hemorrhoids: From basic pathophysiology to clinical management. World J Gastroenterol. 2012;18:2009–2017. doi: 10.3748/wjg.v18.i17.2009. DOI: https://doi.org/10.3748/wjg.v18.i17.2009
Simillis C, Thoukididou SN, Slesser AAP, Rasheed S, Tan E, Tekkis PP. Systematic review and network meta-analysis comparing clinical outcomes and effectiveness of surgical treatments for haemorrhoids. Br J Surg. 2015;102:1603–1618. doi: 10.1002/bjs.9913. DOI: https://doi.org/10.1002/bjs.9913
Gallo G, Martellucci J, Sturiale A, Clerico G, Milito G, Marino F, et al. Consensus statement of the Italian society of colorectal surgery (SICCR): management and treatment of hemorrhoidal disease. Tech Coloproctol. 2020;24(2):145-164. doi: 10.1007/s10151-020-02149-1. DOI: https://doi.org/10.1007/s10151-020-02149-1
Ham OK, Kang Y, Teng H, Lee Y, Im EO. Consistency and accuracy of multiple pain scales measured in cancer patients from multiple ethnic groups. Cancer Nurs. 2015;38(4):305-311. doi: 10.1097/NCC.0000000000000179. DOI: https://doi.org/10.1097/NCC.0000000000000179
Safikhani S, Gries KS, Trudeau JJ, Reasner D, Rüdell K, Coons SJ, et al. Response scale selection in adult pain measures: results from a literature review. J Patient Rep Outcomes. 2018;2:40. doi: 10.1186/s41687-018-0053-6. DOI: https://doi.org/10.1186/s41687-018-0053-6
Atisook R, Euasobhon P, Saengsanon A, Jensen MP. Validity and utility of four pain intensity measures for use in international research. J Pain Res. 2021;14:1571–1582. doi: 10.2147/JPR.S312177. DOI: https://doi.org/10.2147/JPR.S303305
Adeboye A, Hart R, Senapathi SH, Ali N, Holman L, Thomas HW. Assessment of functional pain score by comparing to traditional pain scores. Cureus. 2021;13(8):e16847. doi: 10.7759/cureus.16847. DOI: https://doi.org/10.7759/cureus.16847
Tsze DS, Hirschfeld G, Dayan PS, Bulloch B, von Baeyer CL. Defining no pain, mild, moderate, and severe pain based on the Faces Pain Scale-Revised and Color Analog Scale in children with acute pain. Pediatr Emerg Care. 2018;34(8):537-544. doi: 10.1097/PEC.0000000000000791. DOI: https://doi.org/10.1097/PEC.0000000000000791
International Association for the Study of Pain. Faces Pain Scale - Revised. Available from: https://www.iasp-pain.org/resources/faces-pain-scale-revised/
Al-Shamari AL, Assi MH, Al-Abbasi M. Anterior knee pain (AKP) and its relationship to quadriceps angle and anthropometric parameters: A hospital-based cross-sectional study from Iraq. Med J Babylon. 2024;21(2):353–358. doi: 10.4103/MJBL.MJBL_739_23. DOI: https://doi.org/10.4103/MJBL.MJBL_739_23
International Association for the Study of Pain. Faces Pain Scale – Revised home. 2018. Available from: https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1519.
Assi MH. Gender determination using hand parameters: A cross-sectional analytical study in Iraq. Al-Rafidain J Med Sci. 2023;5(1S):S23–S28. doi: 10.54133/ajms.v5i1S.301. DOI: https://doi.org/10.54133/ajms.v5i1S.301
Laibee AR, Akkila SS, Khamees N, Eleiwe SA, Salem YG. Short-term effects of laparoscopic sleeve gastrectomy on anatomical and biochemical parameters in morbidly obese Iraqi patients. Bali Med J. 2021;10(3):1045–1049. doi: 10.15562/bmj.v10i3.2615. DOI: https://doi.org/10.15562/bmj.v10i3.2615
Eleiwe SA. Does neonatal Apgar score affect chronological factor in postpartum uterine involution? Life Sci J. 2013;10(11).
Laibee AR, Eleiwe SA. Selected cases of liver mass's surgeries and postoperative complications: A retrospective study in Iraqi samples. Ann Rom Soc Cell Biol. 2021;25(6).
Al-Ameri LT, Shukri ME, Hameed EK, Marzook AA. Pregabalin versus gabapentin efficacy in the management of neuropathic pain associated with failed back surgery syndrome. J Korean Neurosurg Soc. 2024;67(2):202–208. doi: 10.3340/jkns.2022.0225. DOI: https://doi.org/10.3340/jkns.2022.0225
Uten T, Chesnais M, van de Velde M, Raeder J, Beloeil H.. Pain management after open colorectal surgery: An update of the systematic review and procedure-specific postoperative pain management (PROSPECT) recommendations. Eur J Anaesthesiol. 2024;41(5):363-366. doi: 10.1097/EJA.0000000000001978. DOI: https://doi.org/10.1097/EJA.0000000000001978
Cao B, Xu Q, Shi Y, Zhao R, Li H, Zheng J, et al. Pathology of pain and its implications for therapeutic interventions. Signal Transduct Target Ther. 2024;9(1):155. doi: 10.1038/s41392-024-01845-w. DOI: https://doi.org/10.1038/s41392-024-01845-w
Bikfalvi A, Faes C, Freys SM, Joshi GP, Van de Velde M, Albrecht E. PROSPECT guideline for haemorrhoid surgery: A systematic review and procedure-specific postoperative pain management recommendations. Eur J Anaesthesiol Intensive Care. 2023;2(3):e0023. doi: 10.1097/EA9.0000000000000023. DOI: https://doi.org/10.1097/EA9.0000000000000023
Kehlet H, Dahl JB. The value of "multimodal" or "balanced analgesia" in postoperative pain treatment. Anesth Analg. 1993;77:1048–1056. doi: 10.1213/00000539-199311000-00030. DOI: https://doi.org/10.1213/00000539-199311000-00030
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











