Psychosexual Implications of Tubal Ligation in a Sample of Iraqi Women
DOI:
https://doi.org/10.54133/ajms.v7i1.1178Keywords:
Iraqi women, Psychosexual implications, Tubal ligationAbstract
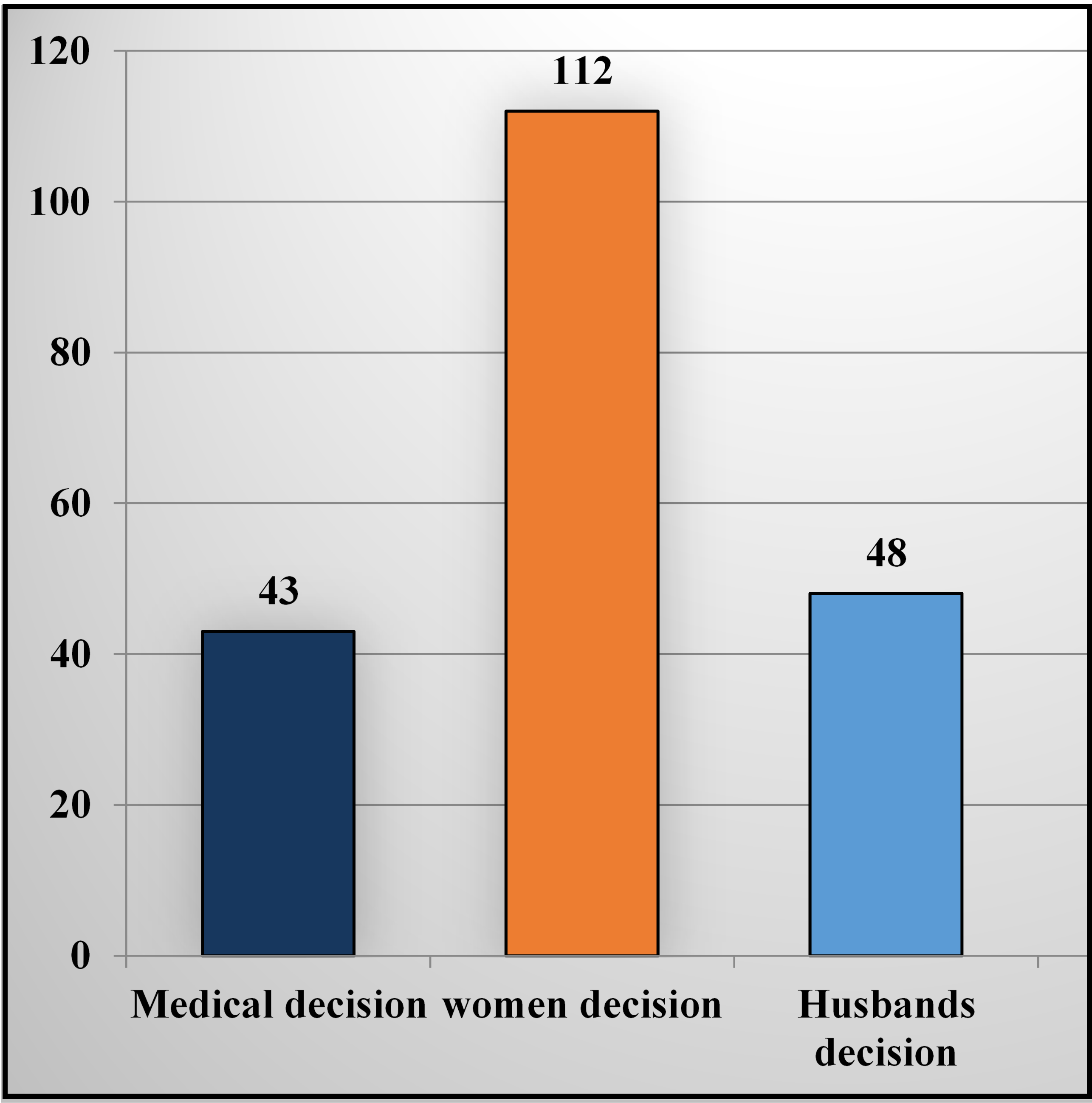
Background: Tubal ligation, recognized as a surgical intervention that ensures permanent contraception, has established itself as an option for women seeking a definitive solution for family planning. Objective: To assess the psychosexual implications of tubal ligation in a sample of women in Baghdad, Iraq. Methods: A prospective cohort study was conducted in a teaching hospital for 2 years, from the first of January 2022 to the end of December 2023, in which 203 women who underwent tubal ligation were included. Results: In the present study, we found that 158 (77.8%) had no depression, mild depression presented in 27 (13.3%), and moderate depression in only 15 (7.4%). While 163 (80.3%) of women did not suffer from anxiety, 32 (15.8%) had mild to moderate anxiety, and only 8 (3.9%) were presented with severe anxiety. 27 (13.3%) have changed in coital frequency this this week. 49 (24.2%) have a change in sexual desire, a change in pleasure, and 37 (18.2%) suffer from a change in orgasm. Conclusions: The current study concluded that there are noticeable psychosexual effects of tubal ligation in women.
Downloads
References
Cash TF, Smolak L, (eds.), Body image: A handbook of science, practice, and prevention. Guilford press; 2011.
Kingsberg SA, Woodard T. Female sexual dysfunction: focus on low desire. Obstet Gynecol. 2015;125(2):477-486. doi: 10.1097/AOG.0000000000000620. DOI: https://doi.org/10.1097/AOG.0000000000000620
DeStefano F, Huezo CM, Peterson HB, Rubin GL, Layde PM, Ory HW. Menstrual changes after tubal sterilization. Obstet Gynecol. 1983;62(6):673-81. PMID: 6633993.
Gentile GP, Kaufman SC, Helbig DW. Is there any evidence for a post-tubal sterilization syndrome? Fertil Steril. 1998;69(2):179-186. doi: 10.1016/s0015-0282(97)00229-x. DOI: https://doi.org/10.1016/S0015-0282(97)00229-X
Taşkömür AT, Erten Ö. The effect of tubal ligation surgery during cesarean operation on dysmenorrhoea, dyspareunia and menstrual cycle. J Gynecol Obstet Hum Reprod. 2021;50(6):102054. doi: 10.1016/j.jogoh.2020.102054. DOI: https://doi.org/10.1016/j.jogoh.2020.102054
Muhamad R, Horey D, Liamputtong P, Low WY, Sidi H. Meanings of sexuality: Views from Malay women with sexual dysfunction. Arch Sex Behav. 2019;48(3):935-947. doi: 10.1007/s10508-018-1228-1. DOI: https://doi.org/10.1007/s10508-018-1228-1
Gulum M, Yeni E, Sahin MA, Savas M, Ciftci H. Sexual functions and quality of life in women with tubal sterilization. Int J Impot Res. 2010;22(4):267-71. doi: 10.1038/ijir.2010.14. DOI: https://doi.org/10.1038/ijir.2010.14
Kunkeri SP, Sathyanarayana Rao TS, Andrade C. Study of sexual functioning and disorder in women before and after tubal sterilization (tubectomy). Indian J Psychiatry. 2017;59(1):63-68. doi: 10.4103/0019-5545.204433. DOI: https://doi.org/10.4103/0019-5545.204433
Ashrafi M, Sadatmahalleh SJ, Mirzaei N, Jahangiri N, Youseflu S, Nasiri M. Comparison of various aspects of women's lives between infertile and women with and without tubal ligation: a comparative cross-sectional study. BMC Womens Health. 2021;21(1):318. doi: 10.1186/s12905-021-01454-7. DOI: https://doi.org/10.1186/s12905-021-01454-7
Khorana AB, Vyas AA. Psychological complications in women undergoing voluntary sterilization by salpingectomy. Br J Psychiatry. 1975;127:67-70. doi: 10.1192/bjp.127.1.67. DOI: https://doi.org/10.1192/bjp.127.1.67
Simonelli C, Eleuteri S, Petruccelli F, Rossi R. Female sexual pain disorders: dyspareunia and vaginismus. Curr Opin Psychiatry. 2014;27(6):406-412. doi: 10.1097/YCO.0000000000000098. DOI: https://doi.org/10.1097/YCO.0000000000000098
Costello C, Hillis SD, Marchbanks PA, Jamieson DJ, Peterson HB. The effect of interval tubal sterilization on sexual interest and pleasure. Obstet Gynecol. 2002;100(3):511-517. doi: 10.1016/s0029-7844(02)02042-2. DOI: https://doi.org/10.1097/00006250-200209000-00018
Pauls RN. Impact of gynecological surgery on female sexual function. Int J Impot Res. 2010;22(2):105-114. doi: 10.1038/ijir.2009.63. DOI: https://doi.org/10.1038/ijir.2009.63
Smith A, Lyons A, Ferris J, Richters J, Pitts M, Shelley J. Are sexual problems more common in women who have had a tubal ligation? A population-based study of Australian women. BJOG. 2010;117(4):463-48. doi: 10.1111/j.1471-0528.2009.02469.x. DOI: https://doi.org/10.1111/j.1471-0528.2009.02469.x
Sánchez-Hernández JA, Rebollo-Ramírez MF, Paulin-Badillo JA, Gómez-Linares C, et al. Bilateral tubal occlusion related to dyspareunia. Rev Fac Med (Mex.). 2011;54(2):4-9.
Jahanian Sadatmahalleh SH, Ziaei S, Kazemnejad A, Mohamadi E. Evaluation of influencing factors on tubal sterilization regret: A cross-sectional study. Int J Fertil Steril. 2018;12(3):200-206. doi: 10.22074/ijfs.2018.5272.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











