The Effects of Mode of Delivery on 5-Minute APGAR Score and Neonatal Outcomes: A Cross-sectional Study in Kirkuk, Iraq
DOI:
https://doi.org/10.54133/ajms.v10i1.2710Keywords:
APGAR score at 5 minutes, Mode of delivery, Neonatal outcomesAbstract
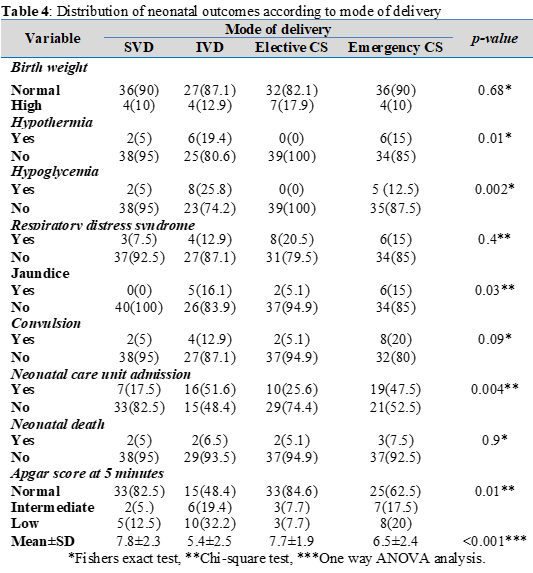
Background: The Apgar score assessed at five minutes serves as a vital measure of a neonate's capacity to survive and thrive. Objective: To assess the relationship between mode of delivery at term and neonatal APGAR score at 5 minutes and neonatal outcomes. Methods: This study was a descriptive cross-sectional study conducted in the labor ward of the department of Obstetrics and Gynecology in Azadi Teaching Hospital, Kirkuk City, Iraq, from 1st of October 2022 to 1st of October 2023. The study sample included 150 pregnant women at term with labor. The mode of delivery was decided by the obstetrician in the labor ward. The APGAR score at 5 minutes and other neonatal outcomes were assessed by the pediatrician in the labor room and followed up for one week after delivery. Results: The mode of delivery was distributed as follows: spontaneous vaginal delivery (26.7%), instrumental vaginal delivery (20.6%), elective cesarean section (26%), and emergency cesarean section (26.7%). The mean APGAR score at 5 minutes for neonates was 7; 12% of them had an intermediate APGAR score, and 17.3% of them had a low APGAR score. The mean APGAR score at 5 minutes was significantly lower in neonates delivered by instrumental vaginal delivery (p<0.001). Conclusions: The mode of delivery, particularly instrumental vaginal delivery, affects the low APGAR score at 5 minutes of neonates.
Downloads
References
Shamsa A, Bai J, Raviraj P, Gyaneshwar R. Mode of delivery and its associated maternal and neonatal outcomes. Open J Obstet Gynecol. 2013;3:307–312. doi: 10.4236/ojog.2013.33057. DOI: https://doi.org/10.4236/ojog.2013.33057
ACOG Practice Bulletin No. 205: Vaginal Birth After Cesarean Delivery. Obstet Gynecol. 2019;133(2):e110-e127. doi: 10.1097/AOG.0000000000003078. DOI: https://doi.org/10.1097/AOG.0000000000003078
ACOG Committee Opinion No. 766: Approaches to Limit Intervention During Labor and Birth. Obstet Gynecol. 2019;133(2):e164-e173. doi: 10.1097/AOG.0000000000003074. DOI: https://doi.org/10.1097/AOG.0000000000003074
National Partnership for Women & Families. Continuous Support for Women During Childbirth: 2017 Cochrane Review Update Key Takeaways. J Perinat Educ. 2018;27(4):193-197. doi: 10.1891/1058-1243.27.4.193. DOI: https://doi.org/10.1891/1058-1243.27.4.193
World Health Organization. WHO statement on cesarean section rates. Geneva: WHO; 2015. Available from: https://apps.who.int/iris/handle/10665/161442
Montoya-Williams D, Lemas DJ, Spiryda L, Patel K, Neu J, Carson TL. What are optimal cesarean section rates in the U.S. and how do we get there? A review of evidence-based recommendations and interventions. J Womens Health (Larchmt). 2017;26(12):1285-1291. doi: 10.1089/jwh.2016.6188. DOI: https://doi.org/10.1089/jwh.2016.6188
Clark RRS, Lake ET. Spontaneous vaginal birth varies significantly across US hospitals. Birth. 2021;48(1):44-51. doi: 10.1111/birt.12508. DOI: https://doi.org/10.1111/birt.12508
Ali UA, Norwitz ER. Vacuum-assisted vaginal delivery. Rev Obstet Gynecol. 2009;2(1):5-17. PMID: 19399290.
Ameh CA, Weeks AD. The role of instrumental vaginal delivery in low resource settings. BJOG. 2009;116(Suppl 1):22-25. doi: 10.1111/j.1471-0528.2009.02331.x. DOI: https://doi.org/10.1111/j.1471-0528.2009.02331.x
Kadas A, Aliyu L, Hauwa M. Instrumental vaginal delivery in bauchi, northeast Nigeria. J West Afr Coll Surg. 2011;1(4):18-27. PMID: 25452969.
Aliya I, Aisha HK, Javaria NM. Vacuum and forceps deliveries; comparison of maternal and neonatal complications. Prof Med J. 2008;15(1):87–90. doi: 10.29309/TPMJ/2008.15.01.2702. DOI: https://doi.org/10.29309/TPMJ/2008.15.01.2702
Eogan M, O’Herlihy C. Guidelines for monitoring the availability and use of obstetric services. New York: UNICEF, WHO, UNFPA; 1997.
Berghella V, Baxter JK, Chauhan SP. Evidence-based surgery for cesarean delivery. Am J Obstet Gynecol. 2005;193(5):1607-1617. doi: 10.1016/j.ajog.2005.03.063. DOI: https://doi.org/10.1016/j.ajog.2005.03.063
Rafiei M, Saei Ghare M, Akbari M, Kiani F, Sayehmiri F, Sayehmiri K, et al. Prevalence, causes, and complications of cesarean delivery in Iran: A systematic review and meta-analysis. Int J Reprod Biomed. 2018;16(4):221-234. PMID: 29942930. DOI: https://doi.org/10.29252/ijrm.16.4.221
Barber EL, Lundsberg LS, Belanger K, Pettker CM, Funai EF, Illuzzi JL. Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol. 2011;118(1):29-38. doi: 10.1097/AOG.0b013e31821e5f65. DOI: https://doi.org/10.1097/AOG.0b013e31821e5f65
Boyle A, Reddy UM, Landy HJ, Huang CC, Driggers RW, Laughon SK. Primary cesarean delivery in the United States. Obstet Gynecol. 2013;122(1):33-40. doi: 10.1097/AOG.0b013e3182952242. DOI: https://doi.org/10.1097/AOG.0b013e3182952242
Singh N, Pradeep Y, Jauhari S. Indications and determinants of cesarean section: A cross-sectional study. Int J Appl Basic Med Res. 2020;10(4):280-285. doi: 10.4103/ijabmr.IJABMR_3_20. DOI: https://doi.org/10.4103/ijabmr.IJABMR_3_20
Lavender T, Hofmeyr GJ, Neilson JP, Kingdon C, Gyte GM. Caesarean section for non-medical reasons at term. Cochrane Database Syst Rev. 2012;(3):CD004660. doi: 10.1002/14651858.CD004660.pub3. DOI: https://doi.org/10.1002/14651858.CD004660.pub3
Habib HA, Abdulla MM, Yacoub SE. Knowledge, and preference of mothers delivering at Al-Kadhumyia Teaching Hospital regarding caesarean section and normal vaginal delivery. Iraqi Postgrad Med J. 2011;10(4):512–518.
Jarjees YT. Cesarean section rates at Al-Batool Maternity Teaching Hospital. Al-Kindy Coll Med J. 2011;7(1):1–4.
Shabila NP. Rates and trends in cesarean sections between 2008 and 2012 in Iraq. BMC Pregnancy Childbirth. 2017;17(1):22. doi: 10.1186/s12884-016-1211-6. DOI: https://doi.org/10.1186/s12884-016-1211-6
Anthony CR, Moore M, Hilborne LH, Rooney A, Hickey S, Ryu Y, et al. Health sector reform in the Kurdistan region-Iraq: Primary care management information system, physician dual practice finance reform, and quality of care training. Rand Health Q. 2018;8(2):1. PMID: 30323984. DOI: https://doi.org/10.7249/RR1658.1
Chen HY, Blackwell SC, Chauhan SP. Association between Apgar score at 5 minutes and adverse outcomes among low-risk pregnancies. J Matern Fetal Neonatal Med. 2022;35(7):1344-1351. doi: 10.1080/14767058.2020.1754789. DOI: https://doi.org/10.1080/14767058.2020.1754789
Getachew B, Etefa T, Asefa A, Terefe B, Dereje D. Determinants of low fifth minute Apgar score among newborn delivered in Jimma University Medical Center, Southwest Ethiopia. Int J Pediatr. 2020;2020:9896127. doi: 10.1155/2020/9896127. DOI: https://doi.org/10.1155/2020/9896127
Thavarajah H, Flatley C, Kumar S. The relationship between the five minute Apgar score, mode of birth and neonatal outcomes. J Matern Fetal Neonatal Med. 2018;31(10):1335-1341. doi: 10.1080/14767058.2017.1315666. DOI: https://doi.org/10.1080/14767058.2017.1315666
Zaigham M, Källén K, Olofsson P. Gestational age-related reference values for Apgar score and umbilical cord arterial and venous pH in preterm and term newborns. Acta Obstet Gynecol Scand. 2019;98(12):1618-1623. doi: 10.1111/aogs.13689. DOI: https://doi.org/10.1111/aogs.13689
Priangga B, Ardian M, Budiono. Comparison of the Apgar score of spontaneous vaginal birth and assisted birth. Folia Med Indonesia. 2014;50(2):119–122.
Thakur N, Sunny AK, Gurung R, Banset O, Litorp H, Ashish KC. Rate and neonatal outcomes among instrument-assisted vaginal birth in 12 public hospitals in Nepal. Res Sq. 2020. Preprint. doi: 10.21203/rs.3.rs-23838/v1. DOI: https://doi.org/10.21203/rs.3.rs-23838/v1
Paudyal L. Comparison of Apgar score of newborns with mode of delivery and its associated factors. Int J Soc Sci Manag. 2020;7(3):176–82. doi: 10.3126/ijssm.v7i3.29961. DOI: https://doi.org/10.3126/ijssm.v7i3.29961
Tarimo CS, Bhuyan SS, Zhao Y, Ren W, Mohammed A, Li Q, et al. Prediction of low Apgar score at five minutes following labor induction intervention in vaginal deliveries: machine learning approach for imbalanced data at a tertiary hospital in North Tanzania. BMC Pregnancy Childbirth. 2022;22(1):275. doi: 10.1186/s12884-022-04534-0. DOI: https://doi.org/10.1186/s12884-022-04534-0
Mohammed EA. Postpartum maternal and neonatal outcomes of SARS-CoV-2 infection during pregnancy. Al-Rafidain J Med Sci. 2023;5:67–72. doi: 10.54133/ajms.v5i.159. DOI: https://doi.org/10.54133/ajms.v5i.159
Mohammed EA, Haseeb MF. Maternal and neonatal outcomes of gestational thrombocytopenia in pregnant women from Kirkuk City, Iraq: A case-control study. Al-Rafidain J Med Sci. 2023;5(Suppl 1): S142-146. doi: 10.54133/ajms.v5i1S.324. DOI: https://doi.org/10.54133/ajms.v5i1S.324
Peters LL, Thornton C, de Jonge A, Khashan A, Tracy M, Downe S, et al. The effect of medical and operative birth interventions on child health outcomes in the first 28 days and up to 5 years of age: A linked data population-based cohort study. Birth. 2018;45(4):347-357. doi: 10.1111/birt.12348. DOI: https://doi.org/10.1111/birt.12348
Ramzan M, Razzaq A, Kiyani AN. Hypoglycemia in small for gestational age neonates based on gestational age, gender, birth weight and mode of delivery. PAFMJ. 2017;67(3):397–400.
Naghipour A, Mostafa Gharebaghi M, Alizadeh H, Fadaee M. The study of association of delivery mode on neonatal jaundice in Al-Zahra and Children’s hospitals of Tabriz in the first 6 months of 1395: cross-sectional. Med J Tabriz Univ Med Sci Health Serv. 2020;41(6):83–90. doi: 10.34172/mj.2020.010. DOI: https://doi.org/10.34172/mj.2020.010
Choudhary B, Choudhary Y, Pakhare AP, Mahto D, Chaturvedula L. Early neonatal outcome in caesarean section: A developing country perspective. Inn J Pediatr. 2016;27(1):e7948. doi: 10.5812/ijp.7948. DOI: https://doi.org/10.5812/ijp.7948
Farhat A, Hafizi L, Pourhoseini MT, Halim F, Mohammadzadeh A, Saeidi R. Comparison of bilirubin level in term infants born by vaginal delivery and cesarean section. Iran J Neonatol. 2016:7(4):45-49. doi: 10.22038/ijn.2016.7189.
Khasawneh W, Obeidat N, Yusef D, Alsulaiman JW. The impact of cesarean section on neonatal outcomes at a university-based tertiary hospital in Jordan. BMC Pregnancy Childbirth. 2020;20(1):335. doi: 10.1186/s12884-020-03027-2. DOI: https://doi.org/10.1186/s12884-020-03027-2
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2026 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











