The Association Between Melasma and Thyroid Dysfunction: A Case-Control Study
DOI:
https://doi.org/10.54133/ajms.v10i1.2669Keywords:
Endocrine dysfunction , Free T4, Melasma, Pigmentation, Thyroid hormones, TSHAbstract
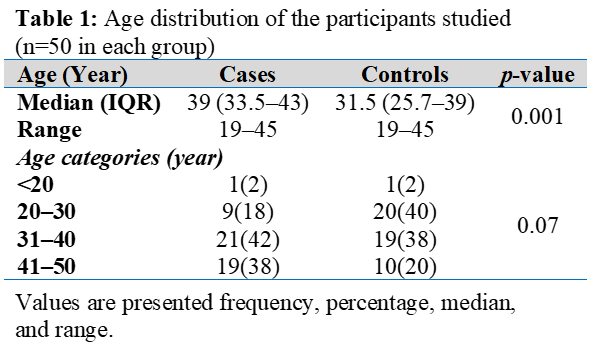
Background: Melasma is a common pigmentary disorder predominantly affecting women. Thyroid hormones influence skin homeostasis and melanocyte activity, suggesting a possible link with melasma. Objective: To investigate the relationship between thyroid hormone levels and melasma in women. Methods: A case-control study was conducted with 100 women aged 18–45 years, including 50 patients with melasma and 50 healthy controls. Free triiodothyronine (T3), free thyroxine (T4), and thyroid-stimulating hormone (TSH) levels in the blood were evaluated in both the clinic and the lab. Results: Women with melasma were significantly older than controls (p=0.001). Compared to controls, melasma patients had lower median free T3 [3.0 (2.6–3.6) vs. 3.3 (3.2–3.5); p=0.02] and free T4 [1.3 (1.1–1.5) vs. 1.4 (1.3–1.4); p=0.001] and higher TSH levels [3.7 (2.8–4.2) vs. 2.2 (1.9–2.5); p=0.001]. These differences remained significant after adjusting for age. Overt thyroid dysfunction was uncommon and not significantly different between groups (p=0.35). Conclusions: Subclinical alterations in thyroid hormones may be associated with melasma in women, independent of age, although causation cannot be established.
Downloads
References
Basit H, Godse KV, Al Aboud AM. Melasma. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459271/
Jo JY, Chae SJ, Ryu HJ. Update on melasma treatments. Ann Dermatol. 2024;36:125. doi: 10.5021/ad.23.133 DOI: https://doi.org/10.5021/ad.23.133
Shahid MA, Ashraf MA, Sharma S. Physiology, thyroid hormone. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.
Cohen B, Cadesky A, Jaggi S. Dermatologic manifestations of thyroid disease: a literature review. Front Endocrinol (Lausanne). 2023;14:1167890. doi: 10.3389/fendo.2023.1167890. DOI: https://doi.org/10.3389/fendo.2023.1167890
Çakmak SK, Özcan N, Kılıç A, Koparal S, Artüz F, Çakmak A, Köse K. Etiopathogenetic factors, thyroid functions and thyroid autoimmunity in melasma patients. Postepy Dermatol Alergol. 2015;32(5):327-330. doi: 10.5114/pdia.2015.54742. DOI: https://doi.org/10.5114/pdia.2015.54742
Rostami Mogaddam M, Iranparvar Alamdari M, Maleki N, Safavi Ardabili N, Abedkouhi S. Evaluation of autoimmune thyroid disease in melasma. J Cosmet Dermatol. 2015;14(2):167-171. doi: 10.1111/jocd.12138. DOI: https://doi.org/10.1111/jocd.12138
Kheradmand M, Afshari M, Damiani G, Abediankenari S, Moosazadeh M. Melasma and thyroid disorders: a systematic review and meta-analysis. Int J Dermatol. 2019;58(11):1231-1238. doi: 10.1111/ijd.14497. DOI: https://doi.org/10.1111/ijd.14497
Tekou A, Labbene I. Association of melasma with thyroid disorders. Sch J Appl Med Sci. 2023;11:1736–1742. doi: 10.36347/sjams.2023.v11i09.024. DOI: https://doi.org/10.36347/sjams.2023.v11i09.024
Proietti I, Battilotti C, Svara F, Innocenzi C, Spagnoli A, Potenza C. Efficacy and tolerability of a microneedling device plus exosomes for treating melasma. Appl Sci. 2024;14(16):7252. doi: 10.3390/app14167252. DOI: https://doi.org/10.3390/app14167252
Al-Ansare NJH, Khine TH. The Relationship between melasma and thyroid dysfunction—analyzing anti-thyroid peroxidase antibody profiles: An immuno-dermatological perspective. Al-Rafidain J Med Sci. 2025;9(2):290- 295. doi: doi: 10.54133/ajms.v9i2.2558. DOI: https://doi.org/10.54133/ajms.v9i2.2558
Espósito ACC, Cassiano DP, da Silva CN, Lima PB, Dias JAF, Hassun K, et al. Update on Melasma-Part I: Pathogenesis. Dermatol Ther (Heidelb). 2022;12(9):1967-1988. doi: 10.1007/s13555-022-00779-x. DOI: https://doi.org/10.1007/s13555-022-00779-x
Handel AC, Miot LDB, Miot HA. Melasma: a clinical and epidemiological review. Bras Dermatol. 2014; 89:771–782. doi; 10.1590/abd1806-4841.20143063. DOI: https://doi.org/10.1590/abd1806-4841.20143063
Suman Babu PS, Sridevi Patil C. Melasma and thyroid profile: a case-control study. IP Indian J Clin Exp Dermatol. 2020;6:76–78. doi: 10.18231/j.ijced.2020.017. DOI: https://doi.org/10.18231/j.ijced.2020.017
Achar A, Rathi SK. Melasma: A clinico-epidemiological study of 312 cases. Indian J Dermatol. 2011;56:380–382. doi: 10.4103/0019-5154.84722. DOI: https://doi.org/10.4103/0019-5154.84722
Liu W, Chen Q, Xia Y. New mechanistic insights of melasma. Clin Cosmet Investig Dermatol. 2023;16:429–442. doi: 10.2147/CCID.S396272. DOI: https://doi.org/10.2147/CCID.S396272
Prabha N, Mahajan VK, Mehta KS, Chauhan PS, Gupta M. Cosmetic contact sensitivity in patients with melasma: results of a pilot study. Dermatol Res Pract. 2014;2014:316219. doi: 10.1155/2014/316219. DOI: https://doi.org/10.1155/2014/316219
Hexsel D, Lacerda DA, Cavalcante AS, Machado Filho CA, Kalil CL, Ayres EL, et al. Epidemiology of melasma in Brazilian patients: a multicenter study. Int J Dermatol. 2014;53(4):440-444. doi: 10.1111/j.1365-4632.2012.05748.x. DOI: https://doi.org/10.1111/j.1365-4632.2012.05748.x
Tamega Ade A, Miot LD, Bonfietti C, Gige TC, Marques ME, Miot HA. Clinical patterns and epidemiological characteristics of facial melasma in Brazilian women. J Eur Acad Dermatol Venereol. 2013;27(2):151-156. doi: 10.1111/j.1468-3083.2011.04430.x. DOI: https://doi.org/10.1111/j.1468-3083.2011.04430.x
Ellerhorst JA, Sendi-Naderi A, Johnson MK, Cooke CP, Dang SM, Diwan AH. Human melanoma cells express functional receptors for thyroid-stimulating hormone. Endocr Relat Cancer. 2006;13(4):1269-1277. doi: 10.1677/erc.1.01239. DOI: https://doi.org/10.1677/erc.1.01239
Cooper DS, Biondi B. Subclinical thyroid disease. Lancet. 2012;379(9821):1142–1154. doi: 10.1016/S0140-6736(11)60276-6. DOI: https://doi.org/10.1016/S0140-6736(11)60276-6
Slominski A, Wortsman J, Tobin DJ. The cutaneous serotoninergic/melatoninergic system: securing a place under the sun. FASEB J. 2005;19(2):176–194. doi: 10.1096/fj.04-2079rev. DOI: https://doi.org/10.1096/fj.04-2079rev
Costin GE, Hearing VJ. Human skin pigmentation: melanocytes modulate skin color in response to stress. FASEB J. 2007;21(4):976–994. doi: 10.1096/fj.06-6649rev. DOI: https://doi.org/10.1096/fj.06-6649rev
Al-Shamma YMH, Al-Wakeel HHA, Al-Awadi IJM. The prevalence of thyroid disorders in patients with melasma. Al-Qadisiyah Med J. 2017;12:107–111. doi: 10.28922/qmj.2016.12.21.107-111. DOI: https://doi.org/10.28922/qmj.2016.12.21.107-111
Talaee R, Ghafarpasand I, Masror H. The relationship between melasma and disturbances in the serum level of thyroid hormones and indices. Med J. 2015;2:19–23.
Dogra A, Dua A, Singh P. Thyroid and skin. Indian J Dermatol. 2006;51:96. doi: 10.4103/0019-5154.26927. DOI: https://doi.org/10.4103/0019-5154.26927
Rahman Y, Krisanti RIA, Wisnu W, Sitohang IBS. The comparison between free thyroxine and thyroid-stimulating hormone levels on melasma severity: a cross-sectional study. Maced J Med Sci. 2021;9:426–431. doi: 10.3889/oamjms.2021.5952. DOI: https://doi.org/10.3889/oamjms.2021.5952
Lutfi RJ, Fridmanis M, Misiunas AL, Pafume O, Gonzalez EA, Villemur JA, et al. Association of melasma with thyroid autoimmunity and other thyroidal abnormalities and their relationship to the origin of the melasma. J Clin Endocrinol Metab. 1985;61(1):28-31. doi: 10.1210/jcem-61-1-28. DOI: https://doi.org/10.1210/jcem-61-1-28
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2026 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).