Delayed Presentation of Testicular Seminoma with Normal Biomarkers: A Case Report and Review
DOI:
https://doi.org/10.54133/ajms.v10i1.2515Keywords:
Alpha-fetoprotein, β-HCG , Orchiectomy , Seminoma , Scrotal swelling , UltrasoundAbstract
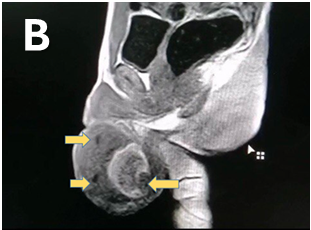
Seminoma is a prominent subtype of testicular cancer, which is the most prevalent solid tumor in young adult males, for the best patient outcome, where early diagnosis and management are crucial. Here we describe a male patient, age 22, who had an RT-sided gradual onset painless scrotal swelling for the last six months. On examination, a hard, well-defined intratesticular mass was felt, which proved to be highly vascular on imaging. Alpha-fetoprotein and β-HCG were within normal range. The provisional diagnosis of seminoma was made, which was confirmed by a histopathological exam, where radical inguinal orchiectomy was performed. The current case emphasizes that although its malignant seminoma produces minimal symptoms, the tumor markers are within normal limits, which adds to the diagnostic challenges. It is important to keep in mind that prompt imaging and surgical management are necessary to achieve better patient outcomes, regardless of normal lab tests. A normal lab test does not exclude malignancy, and the malignant potential has to be kept in mind in the young age group.
Downloads
References
Katabathina VS, Vargas-Zapata D, Monge RA, Nazarullah A, Ganeshan D, Tammisetti V, et al. Testicular germ cell tumors: classification, pathologic features, imaging findings, and management. Radiographics. 2021;41(6):1698–1716. doi: 10.1148/rg.2021210024. DOI: https://doi.org/10.1148/rg.2021210024
Ruf CG, Isbarn H, Wagner W, Fisch M, Matthies C, Dieckmann KP. Changes in epidemiologic features of testicular germ cell cancer: age at diagnosis and relative frequency of seminoma are constantly and significantly increasing. Urol Oncol. 2014;32(1):33. doi: 10.1016/j.urolonc.2012.12.002. DOI: https://doi.org/10.1016/j.urolonc.2012.12.002
Pierre T, Selhane F, Zareski E, Garcia C, Fizazi K, Loriot Y, et al. The role of CT in the staging and follow-up of testicular tumors: baseline, recurrence and pitfalls. Cancers (Basel). 2022;14(16):3965. doi: 10.3390/cancers14163965. DOI: https://doi.org/10.3390/cancers14163965
Tavares NT, Henrique R, Bagrodia A, Jerónimo C, Lobo J. A stroll through the present and future of testicular germ cell tumour biomarkers. Expert Rev Mol Diagn. 2023;23(5):405–418. doi: 10.1080/14737159.2023.2206956. DOI: https://doi.org/10.1080/14737159.2023.2206956
De Visschere P, Bertolotto M, Belfield J, Campo I, Corcioni B, Derchi L, et al. Abdominopelvic imaging in the follow-up of testicular germ-cell tumors in adults: recommendations of the Scrotal and Penile Imaging Working Group of the European Society of Urogenital Radiology. Eur Radiol. 2025:1. doi: 10.1007/s00330-025-11380-z. DOI: https://doi.org/10.1007/s00330-025-11380-z
Sangüesa C, Veiga D, Llavador M, Serrano A. Testicular tumours in children: an approach to diagnosis and management with pathologic correlation. Insights Imaging. 2020;11:1–4. doi: 10.1186/s13244-020-00867-6. DOI: https://doi.org/10.1186/s13244-020-00867-6
Pedrazzoli P, Rosti G, Soresini E, Ciani S, Secondino S. Serum tumour markers in germ cell tumours: From diagnosis to cure. Crit Rev Oncol Hematol. 2021;159:103224. doi: 10.1016/j.critrevonc.2021.103224. DOI: https://doi.org/10.1016/j.critrevonc.2021.103224
Oldenburg J, Berney DM, Bokemeyer C, Climent MA, Daugaard G, Gietema JA, et al. Testicular seminoma and non-seminoma: ESMO-EURACAN Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann Oncol. 2022;33(4):362–375. doi: 10.1016/j.annonc.2022.01.002. DOI: https://doi.org/10.1016/j.annonc.2022.01.002
Murez T, Fléchon A, Branger N, Savoie PH, Rocher L, Camparo P, et al French AFU Cancer Committee Guidelines—Update 2024–2026: Testicular germ cell cancer. French J Urol. 2024;34(12):102718. doi: 10.1016/j.fjurol.2024.102718. DOI: https://doi.org/10.1016/j.fjurol.2024.102718
Bagrodia A, Daneshmand S, Cheng L, Amatruda J, Murray M, Lafin J. The past and future of biomarkers in testicular germ cell tumors. Soc Int Urol J. 2020;1(1):77–84. doi: 10.48083/RZEQ2256. DOI: https://doi.org/10.48083/RZEQ2256
Murray MJ, Huddart RA, Coleman N. The present and future of serum diagnostic tests for testicular germ cell tumours. Nat Rev Urol. 2016;13(12):715–725. doi: 10.1038/nrurol.2016.170. DOI: https://doi.org/10.1038/nrurol.2016.170
Mann K. Tumor markers in testicular cancer. Der Urologe Ausg A. 1990;29(2):77–86. PMID: 2158684.
Gilligan TD, Seidenfeld J, Basch EM, Einhorn LH, Fancher T, Smith DC, et al. ASCO guideline: uses of serum tumor markers in adult males with germ cell tumors. J Clin Oncol. 2010;28(20):3388–3404. doi: 10.1200/JCO.2009.26.4481. DOI: https://doi.org/10.1200/JCO.2009.26.4481
Szymendera JJ, Zborzil J, Sikorowa L, Kamińska JA, Gadek A. Value of five tumor markers (AFP, CEA, hCG, hPL and SP1) in diagnosis and staging of testicular germ cell tumors. Oncology. 1981;38(4):222–229. doi: 10.1159/000225555. DOI: https://doi.org/10.1159/000225555
Aghamir SM, Ghajar HA, Zadeh ZK, Taheri D. Biology of cancer. In: Aghamir SMK, editor. Genetics and Epigenetics of Genitourinary Diseases. Cambridge (MA): Academic Press; 2025. p.181–197. doi: 10.1016/B978-0-443-27302-5.00013-9. DOI: https://doi.org/10.1016/B978-0-443-27302-5.00013-9
Gercek O, Topal K, Yildiz AK, Ulusoy K, Yazar VM. The effect of diagnosis delay in testis cancer on tumor size, tumor stage and tumor markers. Actas Urol Esp. 2024;48(5):356–363. doi: 10.1016/j.acuroe.2023.11.004. DOI: https://doi.org/10.1016/j.acuroe.2023.11.004
Kälin M, Mauti L, Pless M. Testicular cancer: Diagnostics, therapy and follow up. Praxis. 2016;105(11):643–648. doi: 10.1024/1661-8157/a002364. DOI: https://doi.org/10.1024/1661-8157/a002364
Powles T, Bascoul-Mollevi C, Kramar A, Lorch A, Beyer J. Prognostic impact of LDH levels in patients with relapsed/refractory seminoma. J Cancer Res Clin Oncol. 2013;139:1311–1316. doi: 10.1007/s00432-013-1442-0. DOI: https://doi.org/10.1007/s00432-013-1442-0
Singla N, Bagrodia A, Baraban E, Fankhauser CD, Ged YMA. Testicular germ cell tumors: A review. JAMA. 2025;333(9):793–803. doi: 10.1001/jama.2024.27122. DOI: https://doi.org/10.1001/jama.2024.27122
Swadi A, Majid AY, Daraji SD, Mahmood HG. Role of NMP22 and major trace elements in diagnosis of bladder cancer. Ann Trop Med Public Health. 2020;23(S16):SP231605. doi: 10.36295/ASRO.2020.231605. DOI: https://doi.org/10.36295/ASRO.2020.231605
Pang KH, Fallara G, Lobo J, Alnajjar HM, Sangar V, von Stempel C, et al. Management of small testicular masses: a Delphi consensus study. Eur Urol Oncol. 2025;8(1):152–163. doi: 10.1016/j.euo.2024.10.010. DOI: https://doi.org/10.1016/j.euo.2024.10.010
Parekh NV, Lundy SD, Vij SC. Fertility considerations in men with testicular cancer. Transl Androl Urol. 2020;9(Suppl 1):S14–23. doi: 10.21037/tau.2019.08.08. DOI: https://doi.org/10.21037/tau.2019.08.08
Fukunaga H, Yokoya A, Prise KM. A brief overview of radiation-induced effects on spermatogenesis and oncofertility. Cancers (Basel). 2022;14(3):805. doi: 10.3390/cancers14030805. DOI: https://doi.org/10.3390/cancers14030805
D’Costa S, Kotecha P, Rajan P. Lymph node dissection in testicular cancer: Indications and techniques. UroCancer Clin India. 2024;2(3):144–148. doi: 10.4103/UCCI.UCCI_1_25. DOI: https://doi.org/10.4103/UCCI.UCCI_1_25
Okada K, Fujisawa M. Recovery of spermatogenesis following cancer treatment with cytotoxic chemotherapy and radiotherapy. World J Mens Health. 2019;37(2):166–174. doi: 10.5534/wjmh.180043. DOI: https://doi.org/10.5534/wjmh.180043
Patrikidou A, Cazzaniga W, Berney D, Boormans J, de Angst I, Di Nardo D, et al. European Association of Urology guidelines on testicular cancer: 2023 update. Eur Urol. 2023;84(3):289–301. doi: 10.1016/j.eururo.2023.04.010. DOI: https://doi.org/10.1016/j.eururo.2023.04.010
Nori W, Helmi ZR. Can follicular fluid 8-oxo-2’-deoxyguanosine predict the clinical outcomes in ICSI cycle among couples with normospermia male? Obstet Gynecol Sci. 2023;66(5):430. doi: 10.5468/ogs.22170. DOI: https://doi.org/10.5468/ogs.22170
Muhammad Zaki S, Akil Kh Al-Daoody A, Shawket Kawther R. Comparison study in seminal fluid between the cigarette smoker and the non-smoker among infertile males in Erbil city. Kirkuk J Med Sci. 2021;4(1):36–45. doi: 10.32894/kjms.2021.169465. DOI: https://doi.org/10.32894/kjms.2021.169465
Takeshima T, Mimura N, Aoki S, Saito T, Karibe J, Usui K, et al. Pre- and post-chemotherapy spermatogenesis in male patients with malignant bone and soft tissue tumors. Front Pharmacol. 2023;14:1324339. doi: 10.3389/fphar.2023.1324339. DOI: https://doi.org/10.3389/fphar.2023.1324339
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2026 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











