Basic Knowledge About Cervical Cancer and its Screening Tests Among Secondary School Teachers in Baghdad City
DOI:
https://doi.org/10.54133/ajms.v8i1.1759Keywords:
Cervical cancer, HPV, Iraq, Knowledge, Par smear, WomenAbstract
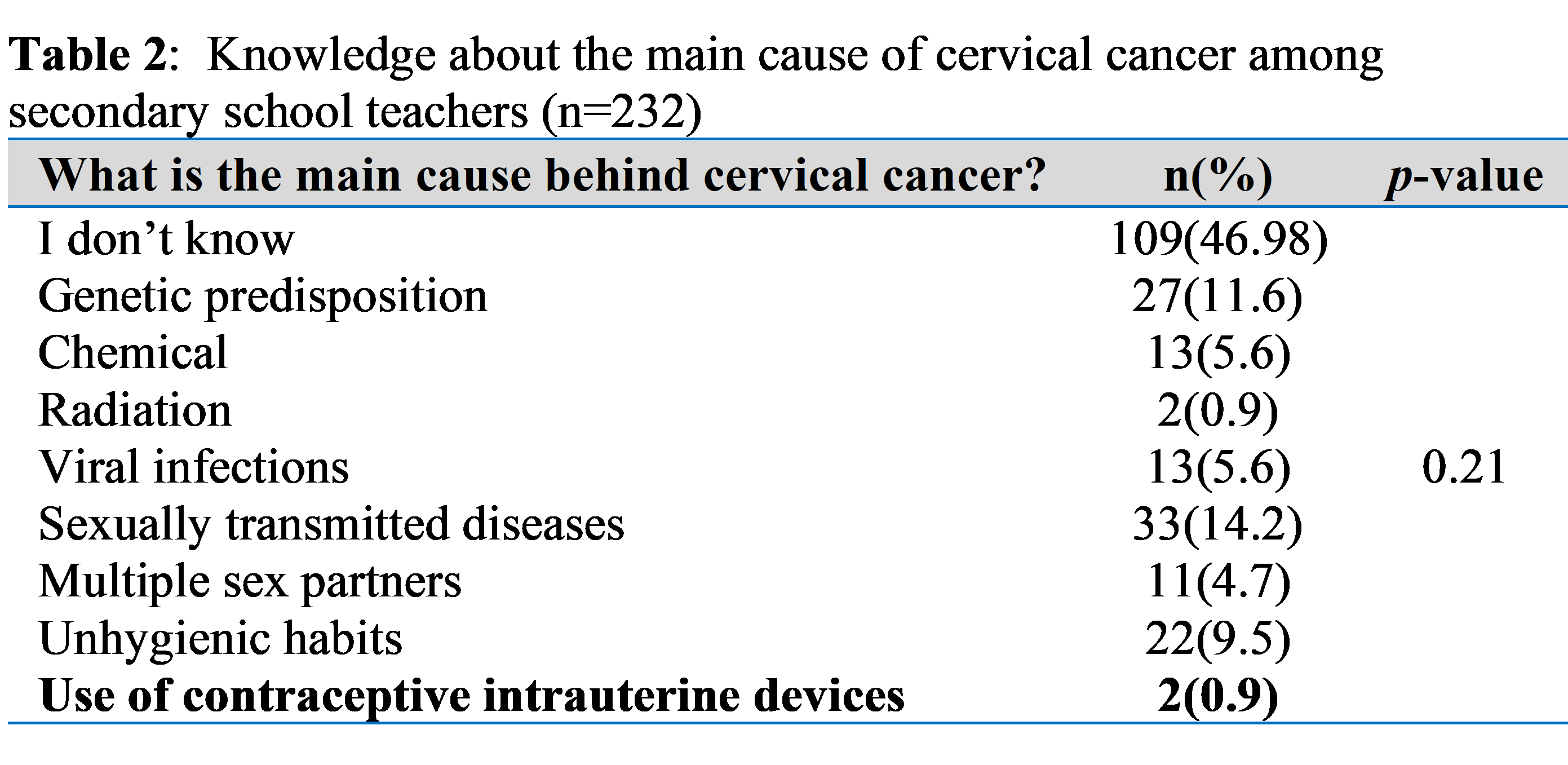
Background: Cervical cancer is a well-defined and preventable major health problem. The main cause behind it is persistent human papillomavirus (HPV) infection. There are more than 200 HPV subtypes, but only a minority of them are oncogenic. The main mode of transmission of this infection is by sexual intercourse. It can be prevented by regular checking for premalignant states by taking cervical smears (Pap smears) and vaccinating young girls. In Iraq, there are no official policies for the preventive measures, and personal awareness is the only way to make women seek screening tests or vaccines. Objectives: To explore the general information of secondary school teachers in Baghdad city/Iraq who are college graduates about cervical cancer. Methods: A cross-sectional study was done, including 232 female secondary school teachers who were interviewed and asked to fill out a written questionnaire. Results: Only 5.6% of the respondents mentioned viral infection as the main cause of cervical cancer, and 14.2% answered a sexually transmitted disease. 14.7% of the teachers included recognize cervical smear as a screening test. Only one teacher (0.4%) knows there is a vaccine to prevent HPV infection. Teaching material mostly has no significant association with the teacher’s information. The main source of information was social media (76.7%). Conclusions: There is poor knowledge about cervical cancer among the educated class, secondary school teachers, and this can affect the rate of occurrence of this preventable disease in the future. Social media can be used to disseminate information regarding cervical cancer among Iraqi women.
Downloads
References
Caruso G, Wagar MK, Hsu HC, Hoegl J, Rey Valzacchi GM, et al. Cervical cancer: a new era. Int J Gynecol Cancer. 2024;34(12):1946-1970. doi: 10.1136/ijgc-2024-005579. DOI: https://doi.org/10.1136/ijgc-2024-005579
Murshid RM, Abdulqader A, Zaidan SA. Exploring the association between chronic endometritis and the risk of endometrial hyperplasia. Bahrain Med Bull. 2024; 46(4):2451-2454.
Kusakabe M, Taguchi A, Sone K, Mori M, Osuga Y. Carcinogenesis and management of human papillomavirus-associated cervical cancer. Int J Clin Oncol. 2023;28(8):965-974. doi: 10.1007/s10147-023-02337-7. DOI: https://doi.org/10.1007/s10147-023-02337-7
Roman BR, Aragones A. Epidemiology and incidence of HPV-related cancers of the head and neck. J Surg Oncol. 2021;124(6):920-922. doi: 10.1002/jso.26687. DOI: https://doi.org/10.1002/jso.26687
Viveros-Carreño D, Fernandes A, Pareja R. Updates on cervical cancer prevention. Int J Gynecol Cancer. 2023;33(3):394-402. doi: 10.1136/ijgc-2022-003703. DOI: https://doi.org/10.1136/ijgc-2022-003703
Milano G, Guarducci G, Nante N, Montomoli E, Manini I. Human papillomavirus epidemiology and prevention: Is there still a gender gap? Vaccines. 2023;11(6):1060. doi: 10.3390/vaccines11061060. DOI: https://doi.org/10.3390/vaccines11061060
Dom-Chima N, Ajang YA, Dom-Chima CI, Biswas-Fiss E, Aminu M, Biswas SB. Human papillomavirus spectrum of HPV-infected women in Nigeria: an analysis by next-generation sequencing and type-specific PCR. Virol J. 2023;20(1):144. doi: 10.1186/s12985-023-02106-y. DOI: https://doi.org/10.1186/s12985-023-02106-y
Vallejo-Ruiz V, Gutiérrez-Xicotencatl L, Medina-Contreras O, Lizano M. Molecular aspects of cervical cancer: a pathogenesis update. Front Oncol. 2024;14:1356581. doi: 10.3389/fonc.2024.1356581. DOI: https://doi.org/10.3389/fonc.2024.1356581
World Health Organization. Cervical cancer , 5 March 2024. Available at: https://www.who.int/news-room/fact-sheets/detail/cervical-cancer
Jensen JE, Becker GL, Jackson JB, Rysavy MB. Human papillomavirus and associated cancers: A review. Viruses. 2024;16(5):680. doi: 10.3390/v16050680. DOI: https://doi.org/10.3390/v16050680
Perkins RB, Wentzensen N, Guido RS, Schiffman M. Cervical cancer screening: A review. JAMA. 2023;330(6):547-558. doi: 10.1001/jama.2023.13174. DOI: https://doi.org/10.1001/jama.2023.13174
Wang J, Elfström KM, Dillner J. Human papillomavirus-based cervical screening and long-term cervical cancer risk: a randomised health-care policy trial in Sweden. Lancet Public Health. 2024;9(11):e886-e895. doi: 10.1016/S2468-2667(24)00218-4. DOI: https://doi.org/10.1016/S2468-2667(24)00218-4
Swanson AA, Pantanowitz L. The evolution of cervical cancer screening. J Am Soc Cytopathol. 2024;13(1):10-15. doi: 10.1016/j.jasc.2023.09.007. DOI: https://doi.org/10.1016/j.jasc.2023.09.007
Siseho KN, Omoruyi BE, Okeleye BI, Okudoh VI, Amukugo HJ, Aboua YG. Women's perception of cervical cancer pap smear screening. Nurs Open. 2022;9(3):1715-1722. doi: 10.1002/nop2.1196. DOI: https://doi.org/10.1002/nop2.1196
Di Fiore R, Suleiman S, Drago-Ferrante R, Subbannayya Y, Pentimalli F, Giordano A, et al. Cancer stem cells and their possible implications in cervical cancer: A short review. Int J Mol Sci. 2022;23(9):5167. doi: 10.3390/ijms23095167. DOI: https://doi.org/10.3390/ijms23095167
Liu L, Wang M, Li X, Yin S, Wang B. An overview of novel agents for cervical cancer treatment by inducing apoptosis: Emerging drugs ongoing clinical trials and preclinical studies. Front Med (Lausanne). 2021;8:682366. doi: 10.3389/fmed.2021.682366. DOI: https://doi.org/10.3389/fmed.2021.682366
Reza S, Anjum R, Khandoker RZ, Khan SR, Islam MR, Dewan SMR. Public health concern-driven insights and response of low- and middle-income nations to the World Health Organization call for cervical cancer risk eradication. Gynecol Oncol Rep. 2024;54:101460. doi: 10.1016/j.gore.2024.101460. DOI: https://doi.org/10.1016/j.gore.2024.101460
Abila DB, Wasukira SB, Ainembabazi P, Kiyingi EN, Chemutai B, Kyagulanyi E, et al. Coverage and socioeconomic inequalities in cervical cancer screening in low- and middle-income countries between 2010 and 2019. JCO Glob Oncol. 2024;10:e2300385. doi: 10.1200/GO.23.00385. DOI: https://doi.org/10.1200/GO.23.00385
WHO Director-General calls for all countries to take action to help end the suffering caused by cervical cancer in 18 May 2018. Available at: https://www.who.int/news/item/18-05-2018-who-dg-calls-for-all-countries-to-take-action-to-help-end-the-suffering-caused-by-cervical-cancer
Saaka SA, Hambali MG. Factors associated with cervical cancer screening among women of reproductive age in Ghana. BMC Women's Health. 2024;24:519. doi: 10.1186/s12905-024-03367-7. DOI: https://doi.org/10.1186/s12905-024-03367-7
Bruni L, Albero G, Serrano B, Mena M, Collado JJ, Gómez D, et al. ICO/IARC information centre on HPV and cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in Iraq. Summary Report 10 March 2023. [Date Accessed]. Available at: https://efaidnbmnnnibpcajpcglclefindmkaj/https://hpvcentre.net/statistics/reports/XWX.pdf
Yousif MG, Al-Amran FG, Sadeq AM, Yousif NG. Prevalence and associated factors of human papillomavirus infection among Iraqi women. Med Adv Innov J. 2023;1(1). Available at: https://efaidnbmnnnibpcajpcglclefindmkaj/https://arxiv.org/pdf/2307.14806
Samari ZJ, Alibraheemi N, Al-Quzweni A, Al- Janabi A, Jumaah AS. (2023). An alarming evidence of increased HPV infection in cervical smear in Iraqi patients. Kufa Med J. 2023;19(1):25-32. doi: 10.36330/kmj.v19i1.11146. DOI: https://doi.org/10.36330/kmj.v19i1.11146
Bitarafan F, Hekmat MR, Khodaeian M, Razmara E, Ashrafganjoei T, Modares Gilani M, et al. Prevalence and genotype distribution of human papillomavirus infection among 12 076 Iranian women. Int J Infect Dis. 2021;111:295-302. doi: 10.1016/j.ijid.2021.07.071. DOI: https://doi.org/10.1016/j.ijid.2021.07.071
Sait KH, Anfinan NM, Sait HK, Basalamah HA. Human papillomavirus prevalence and dynamics: Insights from a 5-year population-based study in Jeddah, Kingdom of Saudi Arabia. Saudi Med J. 2024;45(3):252-260. doi: 10.15537/smj.2024.45.3.20230824. DOI: https://doi.org/10.15537/smj.2024.45.3.20230824
Alwan NA, Al-Attar WM, Al Mallah N, Abdulla KN. (2017). Assessing the knowledge, attitude and practices towards cervical cancer screening among a sample of Iraqi female population. Iraqi J Biotechnol. 2017;16(2):38–47.
Hasan TN, Jwad Taher TM, Ghazi HF. Awareness regarding Pap smear among women in Baghdad city, Iraq. Wiad Lek. 2021;74(9 cz 2):2287-2292. PMID: 34824173. DOI: https://doi.org/10.36740/WLek202109207
Zahid HM, Qarah AB, Alharbi AM, Alomar AE, Almubarak SA. Awareness and practices related to cervical cancer among females in Saudi Arabia. Int J Environ Res Public Health. 2022;19(3):1455. doi: 10.3390/ijerph19031455. DOI: https://doi.org/10.3390/ijerph19031455
Annab A, Lataifeh L, Lataifeh I, Al-Rabadi D, Alkouri O, Khader YS. Factors associated with awareness of and undergoing Pap smear tests among Jordanian women. Narra J. 2024;4(3):e1018. doi: 10.52225/narra.v4i3.1018. DOI: https://doi.org/10.52225/narra.v4i3.1018
Al-Leimon A, Al-Leimon O, Abdulhaq B, Al-Salieby F, Jaber AR, Saadeh M, et al. From awareness to action: Unveiling knowledge, attitudes and testing strategies to enhance human papillomavirus vaccination uptake in Jordan. J Virus Erad. 2024;10(2):100380. doi: 10.1016/j.jve.2024.100380. DOI: https://doi.org/10.1016/j.jve.2024.100380
M Al Kindi R, H Al Sumri H, M Al Muhdhoori T, Al Mamari K, A Al Kalbani M, H Al-Azri M. Knowledge of cervical cancer screening among Omani women attending a university teaching hospital: a cross-sectional study. BMC Womens Health. 2024;24(1):40. doi: 10.1186/s12905-023-02870-7. DOI: https://doi.org/10.1186/s12905-023-02870-7
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











