Psychological Well-Being Intention among Breast Cancer Survivors: A Systematic Literature Review and Walker–Avant Concept Analysis
DOI:
https://doi.org/10.54133/ajms.v10i1.2527Keywords:
Breast cancer survivors, Concept analysis , Psychological well-being , Walker and AvantAbstract
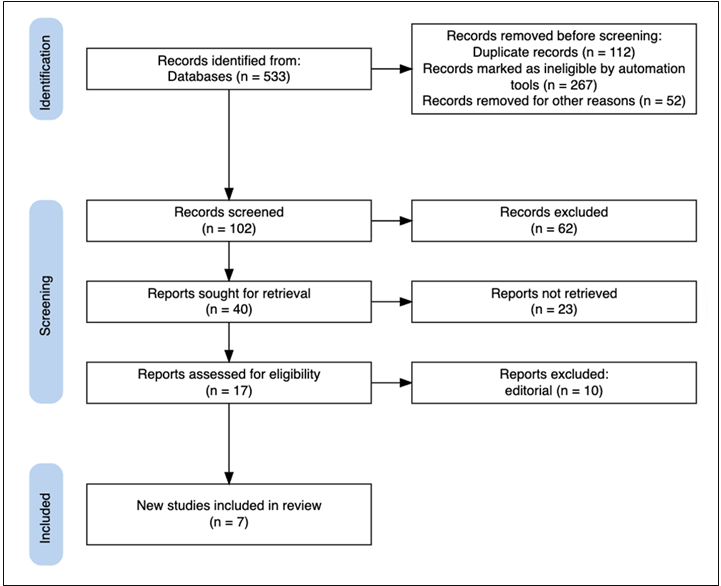
Background: Psychological well-being is crucial for breast cancer survivors, yet psychological well-being remains inconsistently conceptualized in literature and is often treated as a static psychological outcome rather than a dynamic process. Objective: This study aimed to clarify the concept of psychological well-being among breast cancer survivors by identifying its defining attributes, antecedents, consequences, and empirical referents using the Walker and Avant concept analysis framework. Methods: A systematic review of PubMed, ScienceDirect, Google Scholar, and ProQuest was conducted following PRISMA guidelines, and seven articles were analyzed using the Walker and Avant concept analysis method. Results: Psychological well-being intention is conceptualized as a multidimensional, motivational, and adaptive process rather than a passive psychological state. Key attributes include self-acceptance, emotional regulation, adaptive coping, social connectedness, meaning in life, autonomy, and adaptive capacity; antecedents involve illness-related stressors and personal resources, while consequences include positive psychological adaptation, improved quality of life, emotional stability, and treatment engagement. Conclusions: Psychological well-being intention represents an intentional and goal-directed process that underpins survivors’ capacity to adapt to breast cancer as a chronic condition. This clarification offers a theoretical basis for evidence-based interventions to support long-term psychological adaptation in breast cancer survivors.
Downloads
References
WHO. Breast Cancer. Available at: https://www.who.int/news-room/fact-sheets/detail/breast-cancer (2025, accessed 7 November 2025).
Ministry of Health of the Republic of Indonesia. Ministry of Health Performance Report 2024. Jakarta: Ministry of Health of the Republic of Indonesia; 2024. Available at: https://kemkes.go.id/eng/indonesia-health-profile-2024
Pashayan N, Antoniou AC, Ivanus U, Esserman LJ, Easton DF, French D, et al. Personalized early detection and prevention of breast cancer: ENVISION consensus statement. Nat Rev Clin Oncol. 2020 Nov;17(11):687-705. doi: 10.1038/s41571-020-0388-9. DOI: https://doi.org/10.1038/s41571-020-0388-9
Astari AM, Hayati YS, Ar DPA, Laksana K. The experience of breast cancer undergoing chemotherapy. Jurnal Ilmu Kesehatan. 2023;8. doi: 10.30604/jika.v8i2.1528. DOI: https://doi.org/10.30604/jika.v8i2.1528
Rahmadi PMA, Nasution H, Mawar L, Sari M. Pengaruh Kecemasan Terhadap Kepatuhan Pengobatan Kanker Payudara. J Med Nusantara. 2024;2:325–350. DOI: https://doi.org/10.59680/medika.v2i3.1354
Nihayati HE, Jannah WF, Tristiana D. Psychological well-being among breast cancer patients in Surabaya: An overview. Poltekita Jurnal Ilmu Kesehatan. 2025;19: 268–276. doi: 10.33860/jik.v19i2.4160. DOI: https://doi.org/10.33860/jik.v19i2.4160
Widyaningsih S, Istifaraswati A. Psychological well-being of patients with breast cancer: A descriptive study. Sainteks 2019;16. doi: 10.30595/SAINTEKS.V16I2.7125. DOI: https://doi.org/10.30595/sainteks.v16i2.7125
Ministry of Health of the Republic of Indonesia. Ministry of Health Performance Report 2024. Jakarta: Ministry of Health of the Republic of Indonesia; 2024. Available at: https://nsp.mohw.org.tw/data/tmp/20241211/20241211k56cmg.pdf
McKinley, Lauren E, Hua S, Stal J, D’Eon MS, Afari N, et al. Predictors of quality of life among breast cancer patients. California J Health Promot. 2021;19(1):1–12. doi: 10.32398/cjhp.v19i1.2642. DOI: https://doi.org/10.32398/cjhp.v19i1.2642
Annamalai D, Helova A, Saleh M, Gikaara N, Rupani S, Abayo I, et al. Mental health and quality of life following breast cancer diagnosis in patients seen at a tertiary care hospital in Nairobi, Kenya: A qualitative study. Glob Ment Health (Camb). 2024;11:e96. doi: 10.1017/gmh.2024.79. DOI: https://doi.org/10.1017/gmh.2024.79
Han X, Robinson LA, Jensen RE, Smith TG, Yabroff KR. Factors associated with health-related quality of life among cancer survivors in the United States. JNCI Cancer Spectr. 2021;5(1):pkaa123. doi: 10.1093/jncics/pkaa123. DOI: https://doi.org/10.1093/jncics/pkaa123
Lantheaume S, Fernandez L, Lantheaume S, Moták L, Conceição SB. Quality of life in patients with non-metastatic breast cancer: evolution during follow-up and vulnerability factors. Support Care Cancer. 2022;30(3):1935-1943. doi: 10.1007/s00520-021-06203-y. DOI: https://doi.org/10.1007/s00520-021-06203-y
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. DOI: https://doi.org/10.1136/bmj.n71
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, (Eds). Cochrane Handbook for Systematic Reviews of Interventions version 6.5 (updated August 2024). Cochrane, 2024. Available from: www.cochrane.org/handbook.
Tang J, Klunklin P, Lirtmunlikaporn S, Wang Y. Treatment adherence: A concept analysis using the Walker & Avant method. Patient Prefer Adherence. 2024;18:2067-2075. doi: 10.2147/PPA.S477615. DOI: https://doi.org/10.2147/PPA.S477615
Indrayani LND. Trends of concept analysis in nursing science with Walker and Avant approaches: a literature review. Innov Health Soc. 2025;5:51–62. doi: 10.31603/ihs.12858. DOI: https://doi.org/10.31603/ihs.12858
Hancock GR, Stapleton LM, Mueller RO. The Reviewer’s Guide to Quantitative Methods in the Social Sciences, (2nd Ed), 2018; 1–502. DOI: https://doi.org/10.4324/9781315755649
Nasution LA, Ayyanti Y. Self-care among breast cancer survivors: A concept analysis. J Keperawatan Padjadjaran. 2024;12(2):25–32. doi: 10.24198/jkp.v12i2.2504. DOI: https://doi.org/10.24198/jkp.v12i2.2504
Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68-78. doi: 10.1037//0003-066x.55.1.68. DOI: https://doi.org/10.1037//0003-066X.55.1.68
Nipp RD, El-Jawahri A, Fishbein JN, Eusebio J, Stagl JM, Gallagher ER, et al. The relationship between coping strategies, quality of life, and mood in patients with incurable cancer. Cancer. 2016;122(13):2110-2116. doi: 10.1002/cncr.30025. DOI: https://doi.org/10.1002/cncr.30025
Grassi L, Spiegel D, Riba M. Advancing psychosocial care in cancer patients. F1000Res. 2017;6:2083. doi: 10.12688/f1000research.11902.1. DOI: https://doi.org/10.12688/f1000research.11902.1
Caruso R, Nanni MG, Riba MB, Sabato S, Grassi L. The burden of psychosocial morbidity related to cancer: patient and family issues. Int Rev Psychiatry. 2017;29(5):389-402. doi: 10.1080/09540261.2017.1288090. DOI: https://doi.org/10.1080/09540261.2017.1288090
Donovan KA, Grassi L, Deshields TL, Corbett C, Riba MB. Advancing the science of distress screening and management in cancer care. Epidemiol Psychiatr Sci. 2020;29:e85. doi: 10.1017/S2045796019000799. DOI: https://doi.org/10.1017/S2045796019000799
Rodin G. From evidence to implementation: The global challenge for psychosocial oncology. Psychooncology. 2018;27(10):2310-2316. doi: 10.1002/pon.4837. DOI: https://doi.org/10.1002/pon.4837
Smith SK, Loscalzo M, Mayer C, Rosenstein DL. Best practices in oncology distress management: Beyond the screen. Am Soc Clin Oncol Educ Book. 2018;38:813-821. doi: 10.1200/EDBK_201307. DOI: https://doi.org/10.1200/EDBK_201307
Abu-Helalah M, Mustafa H, Alshraideh H, Alsuhail AI, A Almousily O, Al-Abdallah R, et al. Quality of life and psychological wellbeing of breast cancer survivors in the Kingdom of Saudi Arabia. Asian Pac J Cancer Prev. 2022;23(7):2291-2297. doi: 10.31557/APJCP.2022.23.7.2291. DOI: https://doi.org/10.31557/APJCP.2022.23.7.2291
Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol. 1989;57:1069–1081. DOI: https://doi.org/10.1037/0022-3514.57.6.1069
Sharma I, Marwale AV, Sidana R, Gupta ID. Lifestyle modification for mental health and well-being. Indian J Psychiatry. 202;66(3):219-234.
doi:10.4103/indianjpsychiatry.indianjpsychiatry_39_24. DOI: https://doi.org/10.4103/indianjpsychiatry.indianjpsychiatry_39_24
Akel R, El Darsa H, Anouti B, Mukherji D, Temraz S, Raslan R, et al. Anxiety, depression and quality of life in breast cancer patients in the Levant. Asian Pac J Cancer Prev. 2017;18(10):2809-2816. doi: 10.22034/APJCP.2017.18.10.2809.
Abu-Helalah M, Al-Hanaqta M, Alshraideh H, Abdulbaqi N, Hijazeen J. Quality of life and psychological well-being of breast cancer survivors in Jordan. Asian Pac J Cancer Prev. 2014;15(14):5927-5936. doi: 10.7314/apjcp.2014.15.14.5927. DOI: https://doi.org/10.7314/APJCP.2014.15.14.5927
Bò MC, Merlo A, Ligabue MB, Bassi MC, Lusuardi M, Campanini I. Self-managed physical activity in breast cancer survivors: A scoping review. PLoS One. 2023;18(4):e0284807. doi: 10.1371/journal.pone.0284807. DOI: https://doi.org/10.1371/journal.pone.0284807
Subnis UB, Farb NA, Piedalue KL, Speca M, Lupichuk S, Tang PA, et al. A smartphone App-based mindfulness intervention for cancer survivors: Protocol for a randomized controlled trial. JMIR Res Protoc. 2020;9(5):e15178. doi: 10.2196/15178. DOI: https://doi.org/10.2196/15178
Breidenbach C, Heidkamp P, Hiltrop K, Pfaff H, Enders A, Ernstmann N, et al. Prevalence and determinants of anxiety and depression in long-term breast cancer survivors. BMC Psychiatry. 2022;22(1):101. doi: 10.1186/s12888-022-03735-3. DOI: https://doi.org/10.1186/s12888-022-03735-3
Vezzani F, Cabieses B, Obach A, Torrealba S, Carvajal I. Unmet supportive care needs of young women with breast cancer in Chile during follow-up stage after treatment: A qualitative study. PLoS One. 2025;20(8):e0330166. doi: 10.1371/journal.pone.0330166. DOI: https://doi.org/10.1371/journal.pone.0330166
Burkhalter N, Walker SS, Davis M, Flynn A. Integrating primary, behavioral and spiritual health care to improve patient outcomes. J Behav Health Psychol. 2021;10(4):1-8. doi: 10.33425/2832-4579/21033. DOI: https://doi.org/10.33425/2832-4579/21033
Deans C, Carter S. Evidenced interventions supporting the psychological wellbeing of disaster workers: A rapid literature review. Int J Environ Res Public Health. 2025;22(9):1454. doi: 10.3390/ijerph22091454. DOI: https://doi.org/10.3390/ijerph22091454
Purbaningsih ES, Muadi M, Karlina N, Aini CF. An analysis of self-concept and spiritual responses among patients with breast cancer.. Edu Masda J. 2022;6(2):91–102 DOI: https://doi.org/10.52118/edumasda.v6i2.162
Kubzansky LD, Kim ES, Boehm JK, Davidson RJ, Huffman JC, Loucks EB, et al. Interventions to modify psychological well-being: Progress, promises, and an agenda for future research. Affect Sci. 2023;4(1):174-184. doi: 10.1007/s42761-022-00167-w. DOI: https://doi.org/10.1007/s42761-022-00167-w
Sastaviana D, Waji RS. Psychological well-being and readiness for change among employees. Psychopolytan J Psikologi. 2025;9(1):30-38. doi: 10.36341/psi.v9i1.4945. DOI: https://doi.org/10.36341/psi.v9i1.4945
Ryff CD. Psychological well-being revisited: advances in the science and practice of eudaimonia. Psychother Psychosom. 2014;83(1):10-28. doi: 10.1159/000353263. DOI: https://doi.org/10.1159/000353263
Abbott RA, Ploubidis GB, Huppert FA, Kuh D, Croudace TJ. An evaluation of the precision of measurement of Ryff's psychological well-being scales in a population sample. Soc Indic Res. 2010;97(3):357-373. doi: 10.1007/s11205-009-9506-x. DOI: https://doi.org/10.1007/s11205-009-9506-x
Springer KW, Pudrovska T, Hauser RM. Does psychological well-being change with age?: Longitudinal tests of age variations and further exploration of the multidimensionality of Ryff's model of psychological well-being. Soc Sci Res. 2011;40(1):392-398. doi: 10.1016/j.ssresearch.2010.05.008. DOI: https://doi.org/10.1016/j.ssresearch.2010.05.008
Ryff CD, Singer B. Psychological well-being: meaning, measurement, and implications for psychotherapy research. Psychother Psychosom. 1996;65(1):14-23. doi: 10.1159/000289026. DOI: https://doi.org/10.1159/000289026
Dahlem NW, Zimet GD, Walker RR. The Multidimensional scale of perceived social support: A confirmation study. J Clin Psychol. 1991;47(6):756-761. doi: 10.1002/1097-4679(199111)47:6<756::aid-jclp2270470605>3.0.co;2-l. DOI: https://doi.org/10.1002/1097-4679(199111)47:6<756::AID-JCLP2270470605>3.0.CO;2-L
Sulistiani W, Fajrianthi F, Kristiana IF. Validation of the Indonesian version of the multidimensional scale of perceived social support (MSPSS): A Rasch model approach. J Psychol. 2022;21:89–103. doi: 10.14710/jp.21.1.89-103. DOI: https://doi.org/10.14710/jp.21.1.89-103
Zimet GD, Dahlem NW, Zimet SG, Farley GK. (1988). The multidimensional scale of perceived social support. J Pers Assess. 198;52(1):30–41. doi: 10.1207/s15327752jpa5201_2. DOI: https://doi.org/10.1207/s15327752jpa5201_2
Ka ŞC, Şim Şek Çetinkaya Ş. Effect of constructivist model-based adult education on gynaecologic cancer awareness, spiritual well-being, and health anxiety. Health Educ Res. 2025;40(3):cyaf013. doi: 10.1093/her/cyaf013. DOI: https://doi.org/10.1093/her/cyaf013
Ho MH, Lee JJ, Yen HY. Associations between older adults' social media use behaviors and psychosocial well-being. Aging Clin Exp Res. 2023;35(10):2247-2255. doi: 10.1007/s40520-023-02486-9. DOI: https://doi.org/10.1007/s40520-023-02486-9
Anderson RT, Eton DT, Camacho FT, Kennedy EM, Brenin CM, DeGuzman PB, et al. Impact of comorbidities and treatment burden on general well-being among women's cancer survivors. J Patient Rep Outcomes. 2021;5(1):2. doi: 10.1186/s41687-020-00264-z. DOI: https://doi.org/10.1186/s41687-020-00264-z
Yousefi A, Naeimijoo P, Ghadiany M, Lighvan MA, Bakhtiyari M, Arani AM. A randomized control trial of the effectiveness of online Mindfulness-Based Cancer recovery program on psychological wellbeing, caregiver burden and resilience in cancer patients’ caregivers. Med Sci. 2022;26:ms181e2098. doi: 10.54905/disssi/v26i123/ms181e2098. DOI: https://doi.org/10.54905/disssi/v26i123/ms181e2098
Kausar R, Ain Q, Waqar S, Khan MMH, Omar M, Ashraf H. Effects of moderate physical activity on HB level and psychological well-being in females – A randomized control trial. Rehabil J. 2023;7(04):20–25. doi: 10.52567/trehabj.v7i04.44. DOI: https://doi.org/10.52567/trehabj.v7i04.44
Soyer Er Ö, Erkan HN. The mediating role of psychological resilience in the relationship between spiritual well-being and supportive care needs in women with breast cancer. Eur J Breast Health. 2023;19(4):297-303. doi: 10.4274/ejbh.galenos.2023.2023-6-5. DOI: https://doi.org/10.4274/ejbh.galenos.2023.2023-6-5
Guan Z, Zhang Z, Gu K, Wang H, Lin J, Zhou W, et al. Minimally invasive CABG or hybrid coronary revascularization for multivessel coronary diseases: Which is best? A systematic review and metaanalysis. Heart Surg Forum. 2019;22(6):E493-E502. doi: 10.1532/hsf.2499. DOI: https://doi.org/10.1532/hsf.2499
Marisa DE, Dioso R, Elengoe A, Kamasturyan Y, Nurhaeni A. mindfulness-based stress reduction (MBSR) for healthcare workers. Int Res J Multidiscipl Scope. 2025;6:90–96. DOI: https://doi.org/10.47857/irjms.2025.v06i02.02786
Tao L, Lv J, Zhong T, Zeng X, Han M, Fu L, et al. Effects of sleep disturbance, cancer-related fatigue, and psychological distress on breast cancer patients' quality of life: a prospective longitudinal observational study. Sci Rep. 2024;14(1):8632. doi: 10.1038/s41598-024-59214-0. DOI: https://doi.org/10.1038/s41598-024-59214-0
Muzzatti B, Bomben F, Flaiban C, Piccinin M, Annunziata MA. Quality of life and psychological distress during cancer: a prospective observational study involving young breast cancer female patients. BMC Cancer. 2020;20(1):758. doi: 10.1186/s12885-020-07272-8. DOI: https://doi.org/10.1186/s12885-020-07272-8
BCRF. Breast Cancer Statistics And Resources. Breast Cancer Research Foundation, Available at: https://www.bcrf.org/breast-cancer-statistics-and-resources/ (accessed 7 November 2025).
Park S, Sato Y, Takita Y, Tamura N, Ninomiya A, Kosugi T, et al. Mindfulness-based cognitive therapy for psychological distress, fear of cancer recurrence, fatigue, spiritual well-being, and quality of life in patients with breast cancer-A randomized controlled trial. J Pain Symptom Manage. 2020;60(2):381-389. doi: 10.1016/j.jpainsymman.2020.02.017. DOI: https://doi.org/10.1016/j.jpainsymman.2020.02.017
Svendsen K, Nes LS, Meland A, Larsson IM, Gjelsvik YM, Børøsund E, et al. Coping after breast cancer: Protocol for a randomized controlled trial of stress management eHealth interventions. JMIR Res Protoc. 2023;12:e47195. doi: 10.2196/47195. DOI: https://doi.org/10.2196/47195
Alcântara-Silva TR, de Freitas-Junior R, Freitas NMA, de Paula Junior W, da Silva DJ, Machado GDP, et al. Music therapy reduces radiotherapy-induced fatigue in patients with breast or gynecological cancer: A randomized trial. Integr Cancer Ther. 2018;17(3):628-635. doi: 10.1177/1534735418757349. DOI: https://doi.org/10.1177/1534735418757349
Nardin S, Mora E, Varughese FM, D'Avanzo F, Vachanaram AR, Rossi V, Saggia C, et al. Breast cancer survivorship, quality of life, and late toxicities. Front Oncol. 2020;10:864. doi: 10.3389/fonc.2020.00864. DOI: https://doi.org/10.3389/fonc.2020.00864
LaRowe LR, Bohlen LC, Gaudiano BA, Abrantes AM, Butryn ML, Dunsiger SI, et al. Testing the feasibility and acceptability of an acceptance and commitment therapy intervention to increase physical activity among individuals with depression: A protocol paper. Ment Health Phys Act. 2022;23:100475. doi: 10.1016/j.mhpa.2022.100475. DOI: https://doi.org/10.1016/j.mhpa.2022.100475
Waid J, Abusaleh K, Marsalis S. Approaches to strengthen parental self-efficacy: An umbrella review of systematic reviews. Child Youth Serv Rev. 2025;177:108483. doi: 10.1016/j.childyouth.2025.108483. DOI: https://doi.org/10.1016/j.childyouth.2025.108483
Grady PA, Gough LL. Self-management: a comprehensive approach to management of chronic conditions. Am J Public Health. 2014;104(8):e25-31. doi: 10.2105/AJPH.2014.302041. DOI: https://doi.org/10.2105/AJPH.2014.302041
Cáceres MC, Nadal-Delgado M, López-Jurado C, Pérez-Civantos D, Guerrero-Martín J, Durán-Gómez N. Factors related to anxiety, depressive symptoms and quality of life in breast cancer. Int J Environ Res Public Health. 2022;19(6):3547. doi: 10.3390/ijerph19063547. DOI: https://doi.org/10.3390/ijerph19063547
Rezaee M, Darroudi H, Etemad L, Shad AN, Zardast Z, Kohansal H, et al. Anxiety, a significant risk factor for coronary artery disease: what is the best index. BMC Psychiatry. 2024;24(1):443. doi: 10.1186/s12888-024-05798-w. DOI: https://doi.org/10.1186/s12888-024-05798-w
Poulus D, Coulter TJ, Trotter MG, Polman R. Stress and coping in esports and the influence of mental toughness. Front Psychol. 20203;11:628. doi: 10.3389/fpsyg.2020.00628. DOI: https://doi.org/10.3389/fpsyg.2020.00628
Li M, Xie X, Xu H, Li H. A psychological nursing intervention for patients with breast cancer on inflammatory factors, negative emotions and quality of life. Iran J Public Health. 2022;51(9):2041-2047. doi: 10.18502/ijph.v51i9.10559. DOI: https://doi.org/10.18502/ijph.v51i9.10559
Lukka L, Karhulahti VM, Palva JM. Factors affecting digital tool use in client interaction according to mental health professionals: Interview study. JMIR Hum Factors. 2023;10:e44681. doi: 10.2196/44681. DOI: https://doi.org/10.2196/44681
Liu X, Yang M, Ma Y. Living beyond survival: Experiences of self-management among long-term breast cancer survivors – A qualitative study. Int J Nurs Stud Adv. 2026;10:100462. doi: 10.1016/j.ijnsa.2025.100462. DOI: https://doi.org/10.1016/j.ijnsa.2025.100462
Carreira H, Williams R, Dempsey H, Stanway S, Smeeth L, Bhaskaran K. Quality of life and mental health in breast cancer survivors compared with non-cancer controls: a study of patient-reported outcomes in the United Kingdom. J Cancer Surviv. 2021;15(4):564-575. doi: 10.1007/s11764-020-00950-3. DOI: https://doi.org/10.1007/s11764-020-00950-3
Ryff CD, Keyes CL. The structure of psychological well-being revisited. J Pers Soc Psychol. 1995;69(4):719-727. doi: 10.1037//0022-3514.69.4.719. DOI: https://doi.org/10.1037/0022-3514.69.4.719
Beekman E, Verhagen A. Clinimetrics: Hospital anxiety and depression scale. J Physiother. 2018;64(3):198. doi: 10.1016/j.jphys.2018.04.003. DOI: https://doi.org/10.1016/j.jphys.2018.04.003
Kasmad K. Dominant factors contributing to anxiety in triage yellow patients in the emergency department of Ciremai General Hospital: A quantitative multivariate approach. Poltekita: Jurnal Ilmu Kesehatan. 2025;19:193–201. doi: 10.33860/jik.v19i1.4192. DOI: https://doi.org/10.33860/jik.v19i1.4192
Alimohammad HS, Ghasemi Z, Shahriar S, Morteza S, Arsalan K. Effect of hand and foot surface stroke massage on anxiety and vital signs in patients with acute coronary syndrome: A randomized clinical trial. Complement Ther Clin Pract. 2018;31:126-131. doi: 10.1016/j.ctcp.2018.01.012. DOI: https://doi.org/10.1016/j.ctcp.2018.01.012
Wang S, Xia W, Zhang J, Wu M, Tian L. Effects of internet-based mindfulness interventions on anxiety and depression symptoms in cancer patients: A meta-analysis. Gen Hosp Psychiatry. 2025;94:126-141. doi: 10.1016/j.genhosppsych.2025.02.022. DOI: https://doi.org/10.1016/j.genhosppsych.2025.02.022
Lee SC, Moy FM, Hairi NN. Validity and reliability of the Malay version multidimensional scale of perceived social support (MSPSS-M) among teachers. Qual Life Res. 2017;26(1):221-227. doi: 10.1007/s11136-016-1348-9. DOI: https://doi.org/10.1007/s11136-016-1348-9
Laksmita OD, Chung MH, Liao YM, Chang PC. Multidimensional scale of perceived social support in Indonesian adolescent disaster survivors: A psychometric evaluation. PLoS One. 2020;15(3):e0229958. doi: 10.1371/journal.pone.0229958. DOI: https://doi.org/10.1371/journal.pone.0229958
Mubarok F, Miftahuddin M. Psychological well-being scale dengan metode Confirmatory Factor Analysis (CFA). J Pengukuran Psikol dan Pendidikan Indonesia. 2019;7:22–32. DOI: https://doi.org/10.15408/jp3i.v7i1.12105
Saudi NA, Bintang RS, Loloallo VL, Zainuddin NI. Multidimensional scale of perceived social support (MSPSS): Confirmatory factor analysis (CFA). J Ilmu Pendidikan. 2024; 6: 4236–4243. doi: 10.31004/edukatif.v6i4.7492. DOI: https://doi.org/10.31004/edukatif.v6i4.7492
Pancakarsa EP, Soemitro MP, Budianto A, Abdurahman M, Rizki KA, Azhar Y, et al. Analysis of risk factors for psychological stress in breast cancer patients: Observational study in West Java, Indonesia. J Biomed Transl Res. 2024;8(7):4648-4656. doi: 10.37275/bsm.v8i7.1037. DOI: https://doi.org/10.37275/bsm.v8i7.1037
Hajj A, Chamoun R, Salameh P, Khoury R, Hachem R, Sacre H, et al. Fatigue in breast cancer patients on chemotherapy: a cross-sectional study exploring clinical, biological, and genetic factors. BMC Cancer. 2022;22(1):16. doi: 10.1186/s12885-021-09072-0. DOI: https://doi.org/10.1186/s12885-021-09072-0
Getie A, Ayalneh M, Bimerew M. Global prevalence and determinant factors of pain, depression, and anxiety among cancer patients: an umbrella review of systematic reviews and meta-analyses. BMC Psychiatry. 2025;25(1):156. doi: 10.1186/s12888-025-06599-5. DOI: https://doi.org/10.1186/s12888-025-06599-5
Keyes CL. Promoting and protecting mental health as flourishing: a complementary strategy for improving national mental health. Am Psychol. 2007;62(2):95-108. doi: 10.1037/0003-066X.62.2.95. DOI: https://doi.org/10.1037/0003-066X.62.2.95
Keyes CL, Wissing M, Potgieter JP, Temane M, Kruger A, van Rooy S. Evaluation of the mental health continuum-short form (MHC-SF) in setswana-speaking South Africans. Clin Psychol Psychother. 2008;15(3):181-192. doi: 10.1002/cpp.572. DOI: https://doi.org/10.1002/cpp.572
O'Donnell N, Ellis L, Morgan JE, Gregersen PA, Willard V, Howell D, et al. Psychosocial interventions to improve wellbeing in teenage and young adult post-treatment survivors of childhood cancer: A systematic review. Psychooncology. 2025;34(2):e70081. doi: 10.1002/pon.70081. DOI: https://doi.org/10.1002/pon.70081
Ryan RM, Deci EL. On happiness and human potentials: a review of research on hedonic and eudaimonic well-being. Annu Rev Psychol. 2001;52:141-166. doi: 10.1146/annurev.psych.52.1.141. DOI: https://doi.org/10.1146/annurev.psych.52.1.141
McGrady ME, Willard VW, Williams AM, Brinkman TM. Psychological outcomes in adolescent and young adult cancer survivors. J Clin Oncol. 2024;42(6):707-716. doi: 10.1200/JCO.23.01465. DOI: https://doi.org/10.1200/JCO.23.01465
Kim J, Jang M. Stress, social support, and sexual adjustment in married female patients with breast cancer in Korea. Asia Pac J Oncol Nurs. 2019;7(1):28-35. doi: 10.4103/apjon.apjon_31_19. DOI: https://doi.org/10.4103/apjon.apjon_31_19
Sukarnaeni S, Muadi, Marisa DE. Efektivitas terapi relaksasi deep breathing dalam mengurangi ansietas pasien hemodialisis dengan gagal ginjal kronis. Sci J Nurs. 2025;11:403–407. DOI: https://doi.org/10.33023/jikep.v11i3.2619
Siska S, Marisa DE, Purbaningsih ES, Karlina N. Application of deep breathing relaxation technique in hypertensive patients to reduce blood pressure. INDOGENIUS. 2005;4(2A):59–67. doi: 10.56359/igj.v4i2A.717. DOI: https://doi.org/10.56359/igj.v4i2A.717
Diener E, Scollon CN, Lucas RE. The evolving concept of subjective well-being: The multifaceted nature of happiness. In E. Diener (Ed.), Assessing well-being: The collected works of Ed Diener (pp. 67–100). Springer Science + Business Media. 2009. doi: 10.1007/978-90-481-2354-4_4. DOI: https://doi.org/10.1007/978-90-481-2354-4_4
WHO. Health Promotion. Available at: https://www.who.int/teams/health-promotion/enhanced-wellbeing/first-global-conference (accessed 19 February 2025).
Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56(2):267-283. doi: 10.1037//0022-3514.56.2.267. DOI: https://doi.org/10.1037/0022-3514.56.2.267
Zhang C, Zhu R, Lu J, Xue Y, Hou L, Li M, et al. Health promoting lifestyles and influencing factors among empty nesters and non-empty nesters in Taiyuan, China: a cross-sectional study. Health Qual Life Outcomes. 2018;16(1):103. doi: 10.1186/s12955-018-0936-5. DOI: https://doi.org/10.1186/s12955-018-0936-5
Lolokote S, Hidru TH, Li X. Do socio-cultural factors influence college students' self-rated health status and health-promoting lifestyles? A cross-sectional multicenter study in Dalian, China. BMC Public Health. 2017;17(1):478. doi: 10.1186/s12889-017-4411-8. DOI: https://doi.org/10.1186/s12889-017-4411-8
Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: A meta-analytic review. PLoS Med. 2010. doi: 10.1371/JOURNAL.PMED.1000316. DOI: https://doi.org/10.4016/19865.01
Al-Zaben FN, Sehlo MG, Koenig HG. A cross-sectional study of anxiety and marital quality among women with breast cancer at a university clinic in western Saudi Arabia. Saudi Med J. 2015;36(10):1168-1175. doi: 10.15537/smj.2015.10.12254. DOI: https://doi.org/10.15537/smj.2015.10.12254
Gallagher MW, Lopez SJ, Preacher KJ. The hierarchical structure of well-being. J Pers. 2009;77(4):1025-50. doi: 10.1111/j.1467-6494.2009.00573.x. DOI: https://doi.org/10.1111/j.1467-6494.2009.00573.x
Timko Olson ER, Olson A, Driscoll M, Bliss DZ. Psychosocial Factors Affecting Wellbeing and Sources of Support of Young Adult Cancer Survivors: A Scoping Review. Nursing Reports. 2024; 14(4):4006-4021. doi: 10.3390/nursrep14040293. DOI: https://doi.org/10.3390/nursrep14040293
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2026 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











