Exploring the Impact of Systemic Conditions in Shaping Chief Complaints in Iraqi Dental Patients: A Focus on Their Prevalence
DOI:
https://doi.org/10.54133/ajms.v9i2.2405Keywords:
Chief complain, Dental patient, Oral surgery, Systemic condition, Toot extractionAbstract
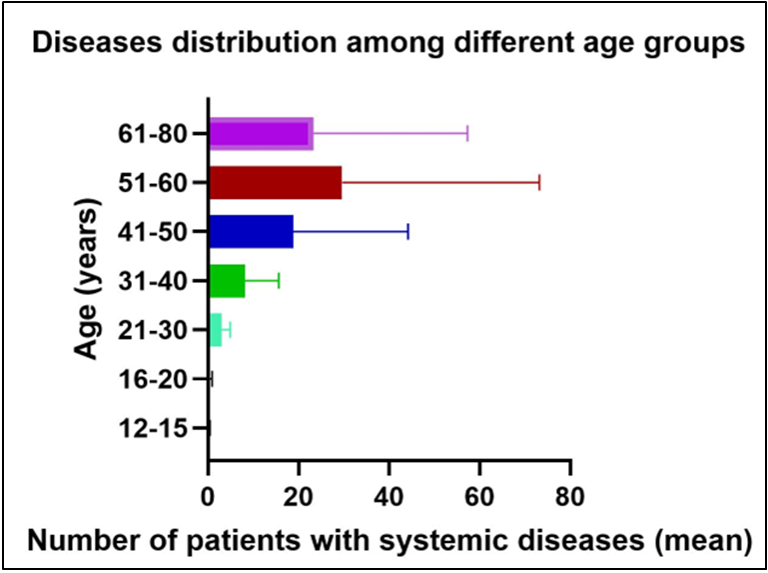
Background: Systemic health conditions can significantly influence oral health and are often associated with tooth loss and specific dental complaints. These diseases may accelerate periodontal breakdown or complicate existing oral conditions, thereby shaping patients' chief complaints and their reasons for seeking dental care. Objective: To assess the impact of systemic conditions on reasons for tooth extraction and evaluate the prevalence of these conditions within the study population. It also documented the most common chief complaints, categorized by gender, age, and systemic conditions. Methods: This prospective cross-sectional study was conducted amongst the Iraqi population, involving a total of 2,581 patients who attended the Oral and Maxillofacial Surgery Department for tooth extraction. Results: The most common chief complaint was a need for prostheses (43%), followed by dental pain (28.4%). Amongst the 2,581 patients, 659(25.5%) had controlled systemic diseases. The most frequently reported condition was hypertension (12.63%), then diabetes (9.33%), thyroid disease (2.24%), ischemic heart disease (2.16%), and respiratory disease (2.05%). A highly significant relationship was observed between diabetes and periodontal diseases, as indicated by the chi-square test (p= 0.004). Conclusions: This study offers the first epidemiological insights into the impact of systemic diseases on the reasons for tooth extractions among the Iraqi population. The findings reveal a significant correlation between specific systemic conditions and oral health issues that ultimately lead to tooth extraction. Additionally, the study underscores the high prevalence of medically compromised individuals.
Downloads
References
Kawachi I, Kennedy BP. Income inequality and health: pathways and mechanisms. Health Serv Res. 1999;34(1 Pt 2):215-227.
Kannan N, Sridevi BS, Manne RK, Sarath P. Medically compromised dental patient: Dentists nightmare. Dent Pract. 2017;14(3):511-517. doi: 10.26717/BJSTR.2017.01.000174. DOI: https://doi.org/10.26717/BJSTR.2017.01.000174
Almas K, Awartani FA. Prevalence of medically compromised patients referred for periodontal treatment to a teaching hospital in Central Saudi Arabia. Saudi Med J. 2003;24(11):1242-1245. PMID: 14647562.
Pavani NPM, Pachava S, Sultana SP, Ravoori S, Rajasekhar P, Talluri D. Impact of diabetes mellitus and other systemic diseases on oral health and tooth mortality. J Family Med Prim Care. 2024;13(1):363-367. doi: 10.4103/jfmpc.jfmpc_1000_23. DOI: https://doi.org/10.4103/jfmpc.jfmpc_1000_23
Usuga-Vacca M, Díaz-Báez D, Beltrán EO, Cortes A, Vargas-Sanchez PK, Avila V. Oral diseases and systemic conditions: correlation analyses from the Colombian national health records between 2016 and 2023. Front Oral Health. 2024;5:1466427. doi: org/10.3389/froh.2024.1466427. DOI: https://doi.org/10.3389/froh.2024.1466427
Chatzopoulos GS, Jiang Z, Marka N, Wolff LF. Periodontal disease, tooth loss, and systemic conditions: An exploratory study. Int Dent J. 2024;74(2):207-215. doi: 10.1016/j.identj.2023.08.002. DOI: https://doi.org/10.1016/j.identj.2023.08.002
Ortarzewska M, Nijakowski K, Jankowski J, Sawicka-Gutaj N, Ruchała M, Surdacka A. Periodontal disease in patients with thyroid diseases: A systematic review with meta-analysis. Adv Med Sci. 2024;69(2):289-295. doi: 10.1016/j.advms.2024.06.003.
Herrera D, Sanz M, Shapira L, Brotons C, Chapple I, Frese T, et al. Periodontal diseases and cardiovascular diseases, diabetes, and respiratory diseases: Summary of the consensus report by the European Federation of Periodontology and WONCA Europe. Eur J Gen Pract. 2024;30(1):2320120. doi: 10.1080/13814788.2024.2320120. DOI: https://doi.org/10.1080/13814788.2024.2320120
Schwarz C, Hajdu AI, Dumitrescu R, Sava-Rosianu R, Bolchis V, Anusca D, et al. Link between oral health, periodontal disease, smoking, and systemic diseases in Romanian patients. Healthcare (Basel). 2023;11(16).. doi: 10.3390/healthcare11162354. DOI: https://doi.org/10.3390/healthcare11162354
Aminoshariae A, Nosrat A, Jakovljevic A, Jaćimović J, Narasimhan S, Nagendrababu V. Tooth loss is a risk factor for cardiovascular disease mortality: a systematic review with meta-analyses. J Endod. 2024. doi: 10.1016/j.joen.2024.06.012. DOI: https://doi.org/10.1016/j.joen.2024.06.012
Sebring D, Buhlin K, Norhammar A, Rydén L, Jonasson P, Lund H, et al. Endodontic inflammatory disease: A risk indicator for a first myocardial infarction. Int Endod J. 2022;55(1):6-17. doi: 10.1111/iej.13634. DOI: https://doi.org/10.1111/iej.13634
Bond JC, McDonough R, Alshihayb TS, Kaye EA, Garcia RI, Heaton B. Edentulism is associated with increased risk of all-cause mortality in adult men. J Am Dent Assoc. 2022;153(7):625-634. doi: 10.1016/j.adaj.2021.11.009. DOI: https://doi.org/10.1016/j.adaj.2021.11.009
Hag Mohamed S, Sabbah W. Is tooth loss associated with multiple chronic conditions? Acta Odontol Scand. 2023;81(6):443-448. doi: 10.1080/00016357.2023.2166986. DOI: https://doi.org/10.1080/00016357.2023.2166986
Hakeem FF, Bernabé E, Sabbah W. Association between oral health and frailty: A systematic review of longitudinal studies. Gerodontology. 2019;36(3):205-215. doi: 10.1111/ger.12406. DOI: https://doi.org/10.1111/ger.12406
Zhu Y, Hollis JH. Tooth loss and its association with dietary intake and diet quality in American adults. J Dent. 2014;42(11):1428-1435. doi: 10.1016/j.jdent.2014.08.012. DOI: https://doi.org/10.1016/j.jdent.2014.08.012
Sheiham A, Nicolau B. Evaluation of social and psychological factors in periodontal disease. Periodontol 2000. 2005;39:118-131. doi: 10.1111/j.1600-0757.2005.00115.x. DOI: https://doi.org/10.1111/j.1600-0757.2005.00115.x
Kudsi Z, Fenlon MR, Johal A, Baysan A. Assessment of psychological disturbance in patients with tooth loss: A systematic review of assessment tools. J Prosthodont. 2020;29(3):193-200. doi: 10.1111/jopr.13141. DOI: https://doi.org/10.1111/jopr.13141
Sampaio-Maia B, Caldas IM, Pereira ML, Pérez-Mongiovi D, Araujo R. The oral microbiome in health and its implication in oral and systemic diseases. Adv Appl Microbiol. 2016;97:171-210. doi: 10.1016/bs.aambs.2016.08.002. DOI: https://doi.org/10.1016/bs.aambs.2016.08.002
Lira-Junior R, Åkerman S, Klinge B, Boström EA, Gustafsson A. Salivary microbial profiles in relation to age, periodontal, and systemic diseases. PLoS One. 2018;13(3):e0189374. doi: 10.1371/journal.pone.0189374. DOI: https://doi.org/10.1371/journal.pone.0189374
Dhanuthai K, Sappayatosok K, Bijaphala P, Kulvitit S, Sereerat T. Prevalence of medically compromised conditions in dental patients. Med Oral Patol Oral Cir Bucal. 2009;14(6):E287-291. PMID: 19300377.
Bhateja S. High prevalence of cardiovascular diseases among other medically compromised conditions in dental patients: A retrospective study. J Cardiovasc Dis Res. 2012;3(2):113-116. doi: 10.4103/0975-3583.95364. DOI: https://doi.org/10.4103/0975-3583.95364
Smeets EC, de Jong KJ, Abraham-Inpijn L. Detecting the medically compromised patient in dentistry by means of the medical risk-related history: A survey of 29,424 dental patients in the Netherlands. Preventive Med. 1998;27(4):530-5. doi: 10.1006/pmed.1998.0285. DOI: https://doi.org/10.1006/pmed.1998.0285
Passarelli PC, Pagnoni S, Piccirillo GB, Desantis V, Benegiamo M, Liguori A, et al. Reasons for tooth extractions and related risk factors in adult patients: A cohort study. Int J Environ Res Public Health. 2020;17(7). doi: 10.3390/ijerph17072575. DOI: https://doi.org/10.3390/ijerph17072575
Alqarni A, AlHarthi S, Felemban M, Abed H, Shukr B, Al-Johani K, et al. The prevalence and patterns of common chief complaints among patients at Taif University Dental Hospital, Saudi Arabia. Saudi J Health Sci. 2024;13:49-55. doi: 10.4103/sjhs.sjhs_136_23. DOI: https://doi.org/10.4103/sjhs.sjhs_136_23
Ikimi NU, Abdullahi S, Ighalo KI, Ojehanon PE. Chief complaint in a dental and maxillofacial surgery department in Abuja Nigeria. Online J Dent Oral Health. 2022;5(3):1. doi: 10.33552/OJDOH.2022.05.000613. DOI: https://doi.org/10.33552/OJDOH.2022.05.000613
Aida J, Ando Y, Akhter R, Aoyama H, Masui M, Morita M. Reasons for permanent tooth extractions in Japan. J Epidemiol. 2006;16(5):214-219. doi: 10.2188/jea.16.214. DOI: https://doi.org/10.2188/jea.16.214
Shooriabi M, Mousavy SM, Ezati M. Evaluation of the knowledge level of dental students regarding the dental management of medically compromised patients. Comprehens Health Biomed Studies. 2023;2(1). doi: 10.5812/chbs-145196. DOI: https://doi.org/10.5812/chbs-145196
Umino M, Nagao M. Systemic diseases in elderly dental patients. Int Dent J. 1993;43(3):213-218. PMID: 8406951.
Li Y, Yuan X, Zheng Q, Mo F, Zhu S, Shen T, et al. The association of periodontal disease and oral health with hypertension, NHANES 2009–2018. BMC Public Health. 2023;23(1):1122. doi: 10.1186/s12889-023-16012-z. DOI: https://doi.org/10.1186/s12889-023-16012-z
Park JH, Kang MK, Leem GH, Kim JW, Song TJ. Chronic periodontal disease is related with newly developing hypertension: a nationwide cohort study. Clin Hypertens. 2024;30(1):27. doi: 10.1186/s40885-024-00285-6. DOI: https://doi.org/10.1186/s40885-024-00285-6
Kimura Y, Tonami KI, Tsuruta J, Araki K. Rise of blood pressure value in young patients at first visit at a dental university hospital in Japan. J Dent Sci. 2019;14(1):93-98. doi: 10.1016/j.jds.2018.11.004. DOI: https://doi.org/10.1016/j.jds.2018.11.004
Yan S, Sha S, Li S, Wang D, Jia Y. Association between hypertension and stroke in US adults in the National Health and Nutrition Examination Surveys (NHANES) 2007 to 2018. Postgrad Med. 2023;135(2):187-194. doi: 10.1080/00325481.2022.2138470. DOI: https://doi.org/10.1080/00325481.2022.2138470
Borgnakke WS, Genco RJ, Eke PI, Taylor GW. Oral Health and Diabetes. In: Cowie CC, Casagrande SS, Menke A, Cissell MA, Eberhardt MS, Meigs JB, et al, (Eds.), Diabetes in America, (3rd ed.), Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases (US); 2018 Aug. CHAPTER 31. PMID: 33651538.
Ortarzewska M, Nijakowski K, Jankowski J, Sawicka-Gutaj N, Ruchała M, Surdacka A. Periodontal disease in patients with thyroid diseases: A systematic review with meta-analysis. Adv Med Sci. 2024;69(2):289-295. doi: 10.1016/j.advms.2024.06.003. DOI: https://doi.org/10.1016/j.advms.2024.06.003
Song E, Park MJ, Kim JA, Roh E, Yu JH, Kim NH, et al. Implication of thyroid function in periodontitis: a nationwide population-based study. Sci Rep. 2021;11(1):22127. doi: 10.1038/s41598-021-01682-9. DOI: https://doi.org/10.1038/s41598-021-01682-9
Dibello V, Lozupone M, Manfredini D, Dibello A, Zupo R, Sardone R, et al. Oral frailty and neurodegeneration in Alzheimer's disease. Neural Regen Res. 2021;16(11):2149-2153. doi: 10.4103/1673-5374.310672. DOI: https://doi.org/10.4103/1673-5374.310672
Rodgers JL, Jones J, Bolleddu SI, Vanthenapalli S, Rodgers LE, Shah K, et al. Cardiovascular risks associated with gender and aging. J Cardiovasc Dev Dis. 2019;6(2). doi: 10.3390/jcdd6020019. DOI: https://doi.org/10.3390/jcdd6020019
Li X, Kolltveit KM, Tronstad L, Olsen I. Systemic diseases caused by oral infection. Clin Microbiol Rev. 2000;13(4):547-558. doi: 10.1128/CMR.13.4.547. DOI: https://doi.org/10.1128/CMR.13.4.547
Blaizot A, Vergnes JN, Nuwwareh S, Amar J, Sixou M. Periodontal diseases and cardiovascular events: meta-analysis of observational studies. Int Dent J. 2009;59(4):197-209. doi: 10.1922/IDJ_2114Sixou13. DOI: https://doi.org/10.1016/S0020-6539(20)33890-9
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).











