Efficacy and Outcome of Oxygen Delivery Devices in Respiratory Distress in Newborn Babies in a Rural Hospital, India
DOI:
https://doi.org/10.54133/ajms.v7i1.1179Keywords:
Biophysical profile, Hypoxia, Heart rate variability, New-born, Nasal injuries, Oxygen delivery devicesAbstract
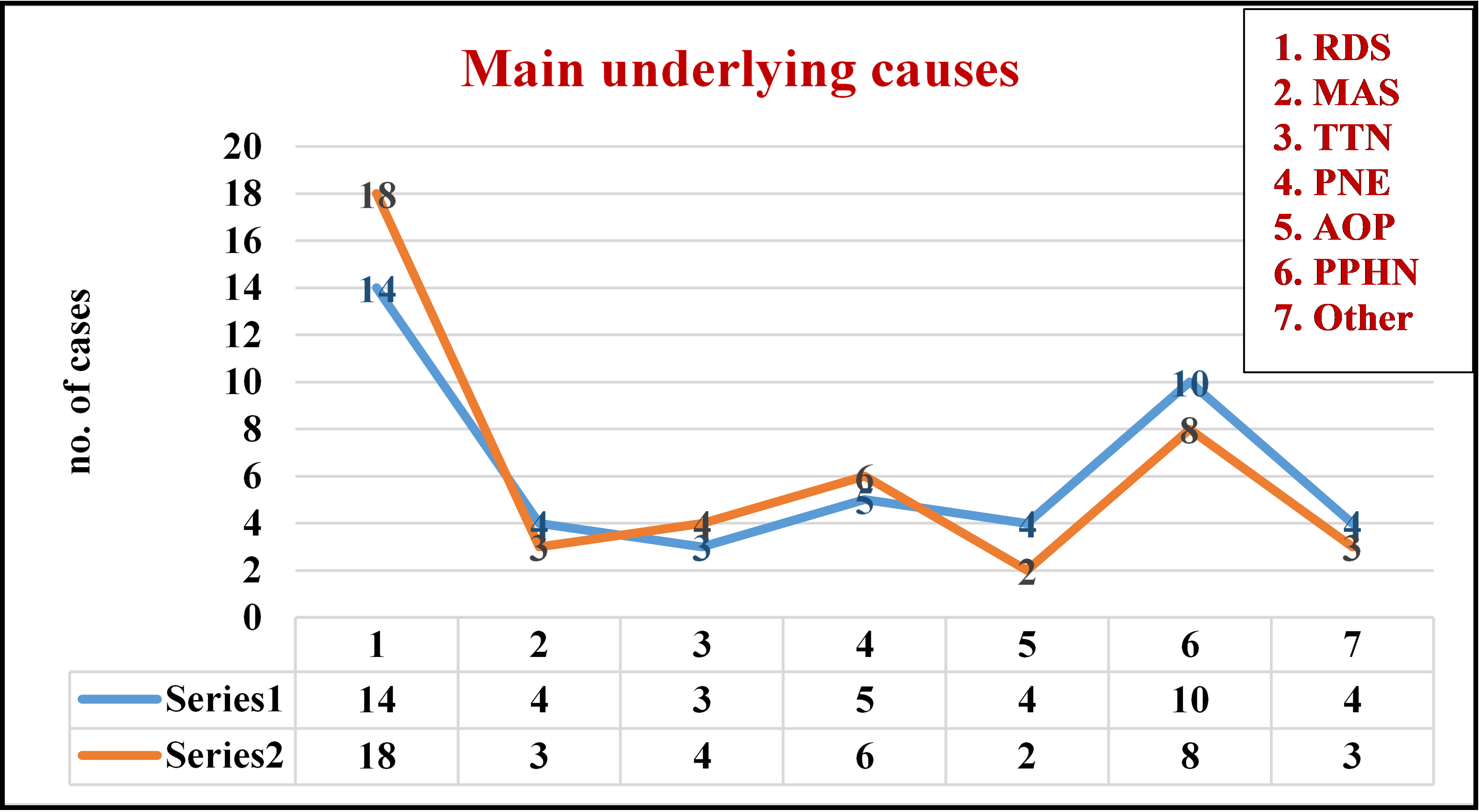
Background: Respiratory distress is a typical presentation in newborn intensive care units, necessitating mechanical ventilation. Once the baby's condition improves, they are put on oxygen therapy. Nasal cannulas and oxygen hoods are the most commonly used and time-tested methods of providing oxygen treatment. Objectives: To assess the efficacy and outcome of these two devices, as well as their impact on several parameters such as desaturation, heart rate, blood gas anomalies, and adverse effects. Methods: This was a prospective, comparative, interventional study conducted in a rural hospital in Sawangi Meghe, Wardha, Maharashtra. Results: Males accounted for 59% of the 88 infants. The majority of newborns had gestational ages between 28 and 32 weeks. Desaturation episodes were more frequent in patients using nasal cannula. In the nasal cannula group, 8 individuals experienced bradycardia, compared to 11 in the oxygen hood. In total, 24 individuals had abnormal blood gas levels. Nasal cannulas were associated with more nose injuries (27.27%) than oxygen hoods (4.5%). Severe-grade injuries were more reported in low birth weight and premature birth patients. The nasal cannula is more convenient and acceptable to nurses. Conclusions: Nasal cannulas may injure the mucosa, yet they are more effective than hoods. Two kinds of oxygen therapy had little effect on heart rate or blood gas levels.
Downloads
References
Sweet DG, Carnielli VP, Greisen G, Hallman M, Klebermass-Schrehof K, Ozek E, et al. European Consensus Guidelines on the Management of Respiratory Distress Syndrome: 2022 Update. Neonatology. 2023;120(1):3-23. doi: 10.1159/000528914. DOI: https://doi.org/10.1159/000528914
Thukral A, Sankar MJ, Chandrasekaran A, Agarwal R, Paul VK. Efficacy and safety of CPAP in low- and middle-income countries. J Perinatol. 2016;36(Suppl 1):S21-S28. doi: 10.1038/jp.2016.29. DOI: https://doi.org/10.1038/jp.2016.29
Jatana SK, Dhingra S, Nair M, Gupta G. Controlled FiO2 therapy to neonates by oxygen hood in the absence of oxygen analyzer. Med J Armed Forces India. 2007;63(2):149-153. doi: 10.1016/S0377-1237(07)80061-X. DOI: https://doi.org/10.1016/S0377-1237(07)80061-X
Tin W, Gupta S. Optimum oxygen therapy in preterm babies. Arch Dis Child Fetal Neonatal Ed. 2007;92(2):F143-F147. doi: 10.1136/adc.2005.092726. DOI: https://doi.org/10.1136/adc.2005.092726
Jobe AH, Kallapur SG. Long-term consequences of oxygen therapy in the neonatal period. Semin Fetal Neonatal Med. 2010;15(4):230-235. doi: 10.1016/j.siny.2010.03.007. DOI: https://doi.org/10.1016/j.siny.2010.03.007
Das A, Mhanna M, Sears J, Houdek JW, Kumar N, Gunzler D, et al. Effect of fluctuation of oxygenation and time spent in the target range on retinopathy of prematurity in extremely low birth weight infants. J Neonatal Perinatal Med. 2018;11(3):257-263. doi: 10.3233/NPM-1757. DOI: https://doi.org/10.3233/NPM-1757
Martin RJ, Wang K, Köroğlu O, Di Fiore J, Kc P. Intermittent hypoxic episodes in preterm infants: do they matter? Neonatology. 2011;100(3):303-310. doi: 10.1159/000329922. DOI: https://doi.org/10.1159/000329922
Frey B, Shann F. Oxygen administration in infants. Arch Dis Child Fetal Neonatal Ed. 2003;88(2):F84-F88. doi: 10.1136/fn.88.2.f84. DOI: https://doi.org/10.1136/fn.88.2.F84
Finer N. Nasal cannula use in the preterm infant: oxygen or pressure? Pediatrics. 2005;116(5):1216-1217. doi: 10.1542/peds.2005-1741. DOI: https://doi.org/10.1542/peds.2005-1741
Jackson JK, Ford SP, Meinert KA, Leick-Rude MK, Anderson B, Sheehan MB, et al. Standardizing nasal cannula oxygen administration in the neonatal intensive care unit. Pediatrics. 2006;118(Suppl 20:S187-196. doi: 10.1542/peds.2006-0913Q. DOI: https://doi.org/10.1542/peds.2006-0913Q
Yllescas-Medrano E, Cordero-González G, Carrera-Muiños S, Mancera-RodrIiguez S. Nasal cannulas versus oxygen hood: success or failure to retire phase II of ventilation (NCPAP or NPV), in premature babies in the neonatal intensive care unit. Perinatol Reprod Hum. 2013;27(3):166-170.
Travers CP, Carlo WA, Nakhmani A, Bhatia S, Gentle SJ, Amperayani VA, et al. Environmental or nasal cannula supplemental oxygen for preterm infants: A randomized cross-over trial. J Pediatr. 2018;200:98-103. doi: 10.1016/j.jpeds.2018.03.010. DOI: https://doi.org/10.1016/j.jpeds.2018.03.010
Fischer C, Bertelle V, Hohlfeld J, Forcada-Guex M, Stadelmann-Diaw C, Tolsa JF. Nasal trauma due to continuous positive airway pressure in neonates. Arch Dis Child Fetal Neonatal Ed. 2010;95(6):F447–F451. doi: 10.1136/adc.2009.179416. DOI: https://doi.org/10.1136/adc.2009.179416
Hensey CC, Hayden E, O'Donnell CP. A randomized crossover study of low-flow air or oxygen via nasal cannulae to prevent desaturation in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2013;98(5):F388-391. doi: 10.1136/archdischild-2012-302623. DOI: https://doi.org/10.1136/archdischild-2012-302623
Woodhead D, Lambert D, Clark J, Christensen R. Comparing two methods of delivering high-flow gas therapy by nasal cannula following endotracheal extubation: a prospective, randomised, masked, crossover trial. J Perinatol. 2006;26:481-485. doi: 10.1038/sj.jp.7211543. DOI: https://doi.org/10.1038/sj.jp.7211543
Parmar J, Pawar V, Warathe A, Singh M, Bajaj R, Kumar J, et al. Rationalizing oxygen usage in a level II special newborn care unit in Madhya Pradesh, India. BMJ Open Qual. 2021;10(Suppl 1):e001386. doi: 10.1136/bmjoq-2021-001386. DOI: https://doi.org/10.1136/bmjoq-2021-001386
A. Pascual, J.M. Wielenga. Nasal pressure injuries among newborns caused by nasal CPAP: An incidence study. J Neonatal Nurs. 2023;29(3):477-481. doi: 10.1016/j. jnn.2022.09.006. DOI: https://doi.org/10.1016/j.jnn.2022.09.006
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).